Monday Poster Session
Category: GI Bleeding
P2084 - Beyond Acquired Von Willebrand Deficiency: Exploring Alternative Mechanisms of Heyde's Syndrome in a Patient with Aortic Stenosis and Angiodysplasia
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Alvin J. Oommen, MD
Montefiore Medical Center
Bronx, NY
Presenting Author(s)
Alvin J. Oommen, MD1, Kripali Gautam, MD2, Akash Kumar, MD1
1Montefiore Medical Center, Bronx, NY; 2NYU Langone Health, New York, NY
Introduction: Heyde's syndrome (HS) is a complex condition characterized by the coexistence of severe aortic stenosis (AS) and gastrointestinal angiodysplasia. The prevailing belief has been that acquired von-Willebrand factor (VWF) deficiency is the underlying cause of HS. However, the validity of this theory remains contentious, as there have been reports of bleeding angiodysplasia in the setting of AS despite normal vWF activity. Here, we present a compelling case of Heyde’s syndrome with negative diagnostic testing for AVWS.
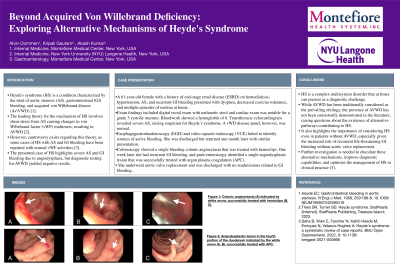
Case Description/Methods: A 61-year-old female with a history of end stage renal disease on hemodialysis, aortic stenosis and a history of recurrent gastrointestinal bleeding presented with dyspnea. Prior to arrival she reported multiple episodes of melena and hematochezia and was found to have a hemoglobin of 6 g/dL. Notable exam findings included melanotic stool on digital rectal exam and a 3/6 systolic crescendo-decrescendo murmur that radiated up to the carotids. A transthoracic echocardiogram demonstrated evidence of severe aortic stenosis with an aortic valve area of 0.9cm2. Considering the recurrent gastrointestinal bleeding and severe AS, Heyde's Syndrome was suspected. To investigate this further, a VWF disease panel was sent, revealing normal levels of VWF antigen (153%), ristocetin co-factor activity (101%), and Factor 8 coagulation assay (191%). Additionally, VWF multimeric analysis revealed a normal multimeric pattern. Given hemodynamic stability, she was discharged, but had multiple readmissions soon after with recurrent GI bleeding requiring endoscopic intervention. On her last visit she underwent TAVR with notable resolution in her GI bleeds thereafter. She had no further readmissions or episodes of GI bleeding on follow up.
Discussion: The prevailing theory regarding the etiology of HS is acquired vWF deficiency (AVWS). However, the validity of this theory remains a topic of debate, as a growing body of evidence suggests that the absence of AVWS does not necessarily rule out the diagnosis. Several alternative theories have been suggested, including mucosal hypoperfusion, alteration of pulse waveforms, and low-grade hypoxia, all of which can be caused by AS and contribute to the development of angioectasia. The absence of AVWS in our patient raises questions about its prevalence in HS and its status as a key feature as well as highlights the importance of considering HS event without AVWS, given the risk of recurrent life-threatening GI bleed.
Disclosures:
Alvin J. Oommen, MD1, Kripali Gautam, MD2, Akash Kumar, MD1. P2084 - Beyond Acquired Von Willebrand Deficiency: Exploring Alternative Mechanisms of Heyde's Syndrome in a Patient with Aortic Stenosis and Angiodysplasia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Montefiore Medical Center, Bronx, NY; 2NYU Langone Health, New York, NY
Introduction: Heyde's syndrome (HS) is a complex condition characterized by the coexistence of severe aortic stenosis (AS) and gastrointestinal angiodysplasia. The prevailing belief has been that acquired von-Willebrand factor (VWF) deficiency is the underlying cause of HS. However, the validity of this theory remains contentious, as there have been reports of bleeding angiodysplasia in the setting of AS despite normal vWF activity. Here, we present a compelling case of Heyde’s syndrome with negative diagnostic testing for AVWS.
Case Description/Methods: A 61-year-old female with a history of end stage renal disease on hemodialysis, aortic stenosis and a history of recurrent gastrointestinal bleeding presented with dyspnea. Prior to arrival she reported multiple episodes of melena and hematochezia and was found to have a hemoglobin of 6 g/dL. Notable exam findings included melanotic stool on digital rectal exam and a 3/6 systolic crescendo-decrescendo murmur that radiated up to the carotids. A transthoracic echocardiogram demonstrated evidence of severe aortic stenosis with an aortic valve area of 0.9cm2. Considering the recurrent gastrointestinal bleeding and severe AS, Heyde's Syndrome was suspected. To investigate this further, a VWF disease panel was sent, revealing normal levels of VWF antigen (153%), ristocetin co-factor activity (101%), and Factor 8 coagulation assay (191%). Additionally, VWF multimeric analysis revealed a normal multimeric pattern. Given hemodynamic stability, she was discharged, but had multiple readmissions soon after with recurrent GI bleeding requiring endoscopic intervention. On her last visit she underwent TAVR with notable resolution in her GI bleeds thereafter. She had no further readmissions or episodes of GI bleeding on follow up.
Discussion: The prevailing theory regarding the etiology of HS is acquired vWF deficiency (AVWS). However, the validity of this theory remains a topic of debate, as a growing body of evidence suggests that the absence of AVWS does not necessarily rule out the diagnosis. Several alternative theories have been suggested, including mucosal hypoperfusion, alteration of pulse waveforms, and low-grade hypoxia, all of which can be caused by AS and contribute to the development of angioectasia. The absence of AVWS in our patient raises questions about its prevalence in HS and its status as a key feature as well as highlights the importance of considering HS event without AVWS, given the risk of recurrent life-threatening GI bleed.
Disclosures:
Alvin Oommen indicated no relevant financial relationships.
Kripali Gautam indicated no relevant financial relationships.
Akash Kumar: Bristol Myers Squibb – Consultant.
Alvin J. Oommen, MD1, Kripali Gautam, MD2, Akash Kumar, MD1. P2084 - Beyond Acquired Von Willebrand Deficiency: Exploring Alternative Mechanisms of Heyde's Syndrome in a Patient with Aortic Stenosis and Angiodysplasia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

