Monday Poster Session
Category: GI Bleeding
P2085 - Recurrent Gastrointestinal Bleeding From an Isolated Ectopic Ileal Varix
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- CT
Christine Tien, MD
Keck School of Medicine of USC
Los Angeles, California
Presenting Author(s)
Christine Tien, MD1, Matthew Rajaratnam, MD1, Alexander Tonthat, MD2, Russell Salamo, MD1, Liyun Yuan, MD, PhD2
1Keck School of Medicine of USC, Los Angeles, CA; 2Keck School of Medicine, University of Southern California, Los Angeles, CA
Introduction: Ectopic variceal hemorrhage is a rare, life-threatening cause of portal hypertensive bleeding that often evades conventional endoscopy, making timely diagnosis and treatment difficult. We present a case of recurrent hematochezia from a covert ileal varix treated with transjugular intrahepatic portosystemic shunt (TIPS).
Case Description/Methods: A 36-year-old woman with alcohol-associated cirrhosis and a ventral hernia was admitted for two days of hematochezia. Her initial blood pressure was 61/31 mmHg. Laboratory studies showed a hemoglobin of 5.4 g/dL, platelets 53 K/cumm, INR 1.84, total bilirubin 2.6 mg/dL. MELD-Na score was 17. EGD showed small nonbleeding esophageal varices without blood in the stomach. The patient had ongoing hematochezia requiring massive transfusion and vasopressor support. A flexible sigmoidoscopy was done in lieu of colonoscopy due to incomplete bowel preparation, which showed active bleeding with fresh blood in the transverse colon but was aborted due to severe tachycardia. A contrast-enhanced CT angiography (CTA) of the abdomen was unremarkable. Interventional radiology performed a mesenteric angiogram without findings of active extravasation. A second CTA revealed a large nonbleeding ileal varix emptying into the superior mesenteric vein favored to represent the source of bleeding. The patient underwent emergent TIPS with resolution of hematochezia. In total, she received 23 units of packed red cells, 3 units of platelets, 6 units of plasma, and 4 pools of cryoprecipitate. She had no further episodes of bleeding at a three week follow-up visit.
Discussion: Our patient underwent several diagnostic measures prior to identification of the culprit varix, highlighting the diagnostic challenge of ectopic varices. Ectopic varices should be considered as sources of obscure gastrointestinal bleeding in patients with portal hypertension. Workup usually includes upper and lower endoscopy followed by exploration of the small intestine with capsule, push, or double balloon enteroscopy and CTA. TIPS should be considered as a first line treatment for ectopic variceal hemorrhage.

Disclosures:
Christine Tien, MD1, Matthew Rajaratnam, MD1, Alexander Tonthat, MD2, Russell Salamo, MD1, Liyun Yuan, MD, PhD2. P2085 - Recurrent Gastrointestinal Bleeding From an Isolated Ectopic Ileal Varix, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Keck School of Medicine of USC, Los Angeles, CA; 2Keck School of Medicine, University of Southern California, Los Angeles, CA
Introduction: Ectopic variceal hemorrhage is a rare, life-threatening cause of portal hypertensive bleeding that often evades conventional endoscopy, making timely diagnosis and treatment difficult. We present a case of recurrent hematochezia from a covert ileal varix treated with transjugular intrahepatic portosystemic shunt (TIPS).
Case Description/Methods: A 36-year-old woman with alcohol-associated cirrhosis and a ventral hernia was admitted for two days of hematochezia. Her initial blood pressure was 61/31 mmHg. Laboratory studies showed a hemoglobin of 5.4 g/dL, platelets 53 K/cumm, INR 1.84, total bilirubin 2.6 mg/dL. MELD-Na score was 17. EGD showed small nonbleeding esophageal varices without blood in the stomach. The patient had ongoing hematochezia requiring massive transfusion and vasopressor support. A flexible sigmoidoscopy was done in lieu of colonoscopy due to incomplete bowel preparation, which showed active bleeding with fresh blood in the transverse colon but was aborted due to severe tachycardia. A contrast-enhanced CT angiography (CTA) of the abdomen was unremarkable. Interventional radiology performed a mesenteric angiogram without findings of active extravasation. A second CTA revealed a large nonbleeding ileal varix emptying into the superior mesenteric vein favored to represent the source of bleeding. The patient underwent emergent TIPS with resolution of hematochezia. In total, she received 23 units of packed red cells, 3 units of platelets, 6 units of plasma, and 4 pools of cryoprecipitate. She had no further episodes of bleeding at a three week follow-up visit.
Discussion: Our patient underwent several diagnostic measures prior to identification of the culprit varix, highlighting the diagnostic challenge of ectopic varices. Ectopic varices should be considered as sources of obscure gastrointestinal bleeding in patients with portal hypertension. Workup usually includes upper and lower endoscopy followed by exploration of the small intestine with capsule, push, or double balloon enteroscopy and CTA. TIPS should be considered as a first line treatment for ectopic variceal hemorrhage.

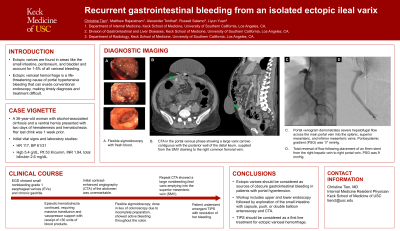
Figure: A. Axial CT through the abdomen in the portal venous phase demonstrates a large varix (arrow) contiguous with the posterior wall of the distal ileum. The varix was supplied by hepatofugal flow from the superior mesenteric vein with cephalad drainage into the right common femoral vein.
B. Portal venogram through a 5 French straight flush catheter demonstrates severe hepatofugal flow across the main portal vein into the splenic, superior mesenteric, and inferior mesenteric veins. Portosystemic gradient was 17 mmHg.
C. Following placement of an 8mm stent from the right hepatic vein to the right portal vein, there is total reversal of flow. The stent has a 6 cm covered intraparenchymal portion and 2 cm uncovered portion in the right portal vein. Portosystemic gradient was calculated at 9 mmHg following stent placement.
B. Portal venogram through a 5 French straight flush catheter demonstrates severe hepatofugal flow across the main portal vein into the splenic, superior mesenteric, and inferior mesenteric veins. Portosystemic gradient was 17 mmHg.
C. Following placement of an 8mm stent from the right hepatic vein to the right portal vein, there is total reversal of flow. The stent has a 6 cm covered intraparenchymal portion and 2 cm uncovered portion in the right portal vein. Portosystemic gradient was calculated at 9 mmHg following stent placement.
Disclosures:
Christine Tien indicated no relevant financial relationships.
Matthew Rajaratnam indicated no relevant financial relationships.
Alexander Tonthat indicated no relevant financial relationships.
Russell Salamo indicated no relevant financial relationships.
Liyun Yuan: Gilead Sciences; Zydus; Intercept; Madrigal pharmaceuticals – Grant/Research Support.
Christine Tien, MD1, Matthew Rajaratnam, MD1, Alexander Tonthat, MD2, Russell Salamo, MD1, Liyun Yuan, MD, PhD2. P2085 - Recurrent Gastrointestinal Bleeding From an Isolated Ectopic Ileal Varix, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

