Monday Poster Session
Category: GI Bleeding
P2098 - Rare Case of Occult Upper Gastrointestinal Bleed Secondary to Duodenal Ampullary Angioectasias
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Rahul R. Thakkar, MD
Baylor Scott & White Health
Round Rock, TX
Presenting Author(s)
Rahul R. Thakkar, MD1, Wasay A. Mohajir, DO2, Erik F. Rahimi, MD2
1Baylor Scott & White Health, Round Rock, TX; 2Baylor Scott & White, Round Rock, TX
Introduction: Angioectasias (AEs) are the most common vascular abnormality in the gastrointestinal (GI) tract. Commonly found in the small intestine, AEs frequently cause overt GI bleeding and warrant an extensive workup. AEs rarely occur in the duodenum, comprising 2.3% of cases in the GI tract. We present a case of an occult GI bleed secondary to multiple bleeding AEs located about the ampulla of Vater, successfully treated with argon plasma coagulation (APC).
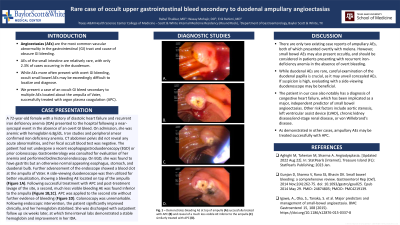
Case Description/Methods: A 72-year-old female with a history of diastolic heart failure and recurrent iron deficiency anemia (IDA) presented to the hospital following a near-syncopal event in the absence of an overt GI bleed. On admission, she was anemic with hemoglobin 6.8g/dL. Iron studies and peripheral smear confirmed iron deficiency anemia. CT abdomen pelvis did not reveal any acute abnormalities, and her fecal occult blood test was negative. The patient had not undergone a recent esophagogastroduodenoscopy (EGD) or prior colonoscopy. Gastroenterology was consulted for evaluation of her anemia and performed bidirectional endoscopy. On EGD, she was found to have gastritis but an otherwise normal appearing esophagus, stomach, and duodenal bulb. Further advancement of the endoscope showed a blood clot at the ampulla of Vater. A side-viewing duodenoscope was then utilized for better visualization, showing a bleeding AE located on top of the ampulla (Figure 1A). Following successful treatment with APC and post-treatment lavage of the site, a second, much less visible bleeding AE was found inferior to the ampulla (Figure 1B,1C). APC was applied to the second site without further evidence of bleeding (Figure 1D). Colonoscopy was unremarkable. Following endoscopic intervention, the patient significantly improved, and her hemoglobin stabilized. She was discharged with outpatient follow up six weeks later, at which time interval labs demonstrated a stable hemoglobin and improvement in her IDA.
Discussion: There are only two existing case reports of ampullary AEs, both of which presented overtly with melena. However, small bowel AEs may also present occultly, and should be considered in patients only presenting with recurrent IDA. While duodenal AEs are rare, careful examination of the duodenal papilla is crucial, as it may unveil concealed AEs. If suspicion is high, evaluating with a side-viewing duodenoscope may be beneficial. As demonstrated in other cases, ampullary AEs may be treated successfully with APC.

Disclosures:
Rahul R. Thakkar, MD1, Wasay A. Mohajir, DO2, Erik F. Rahimi, MD2. P2098 - Rare Case of Occult Upper Gastrointestinal Bleed Secondary to Duodenal Ampullary Angioectasias, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Baylor Scott & White Health, Round Rock, TX; 2Baylor Scott & White, Round Rock, TX
Introduction: Angioectasias (AEs) are the most common vascular abnormality in the gastrointestinal (GI) tract. Commonly found in the small intestine, AEs frequently cause overt GI bleeding and warrant an extensive workup. AEs rarely occur in the duodenum, comprising 2.3% of cases in the GI tract. We present a case of an occult GI bleed secondary to multiple bleeding AEs located about the ampulla of Vater, successfully treated with argon plasma coagulation (APC).
Case Description/Methods: A 72-year-old female with a history of diastolic heart failure and recurrent iron deficiency anemia (IDA) presented to the hospital following a near-syncopal event in the absence of an overt GI bleed. On admission, she was anemic with hemoglobin 6.8g/dL. Iron studies and peripheral smear confirmed iron deficiency anemia. CT abdomen pelvis did not reveal any acute abnormalities, and her fecal occult blood test was negative. The patient had not undergone a recent esophagogastroduodenoscopy (EGD) or prior colonoscopy. Gastroenterology was consulted for evaluation of her anemia and performed bidirectional endoscopy. On EGD, she was found to have gastritis but an otherwise normal appearing esophagus, stomach, and duodenal bulb. Further advancement of the endoscope showed a blood clot at the ampulla of Vater. A side-viewing duodenoscope was then utilized for better visualization, showing a bleeding AE located on top of the ampulla (Figure 1A). Following successful treatment with APC and post-treatment lavage of the site, a second, much less visible bleeding AE was found inferior to the ampulla (Figure 1B,1C). APC was applied to the second site without further evidence of bleeding (Figure 1D). Colonoscopy was unremarkable. Following endoscopic intervention, the patient significantly improved, and her hemoglobin stabilized. She was discharged with outpatient follow up six weeks later, at which time interval labs demonstrated a stable hemoglobin and improvement in her IDA.
Discussion: There are only two existing case reports of ampullary AEs, both of which presented overtly with melena. However, small bowel AEs may also present occultly, and should be considered in patients only presenting with recurrent IDA. While duodenal AEs are rare, careful examination of the duodenal papilla is crucial, as it may unveil concealed AEs. If suspicion is high, evaluating with a side-viewing duodenoscope may be beneficial. As demonstrated in other cases, ampullary AEs may be treated successfully with APC.

Figure: Figure 1: (A) shows intial findings of an actively bleeding ampullary angioectasia. (B) shows results of argon plasma coagulation (APC) on the first lesion with additional bleeding still seen. (C) Shows bleeding emerging from the second angioectasia site, located in the inferior aspect of the ampulla. (D) shows resultant hemostasis after applied APC to the second angioectasia site.
Disclosures:
Rahul Thakkar indicated no relevant financial relationships.
Wasay Mohajir indicated no relevant financial relationships.
Erik Rahimi indicated no relevant financial relationships.
Rahul R. Thakkar, MD1, Wasay A. Mohajir, DO2, Erik F. Rahimi, MD2. P2098 - Rare Case of Occult Upper Gastrointestinal Bleed Secondary to Duodenal Ampullary Angioectasias, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
