Monday Poster Session
Category: IBD
P2123 - Using Quality Improvement Methodology to Develop a Multi-Disciplinary Clinic for Patients With IBD Living in Rural Regions
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Jamie M. Horrigan, MD
Dartmouth-Hitchcock Medical Center
Lebanon, NH
Presenting Author(s)
Jamie M. Horrigan, MD1, Prianca K. Tawde, MD1, Matthew B. Stanton, MD2, Nicola J. Felicetti, RN1, Jessica Salwen-Deremer, PhD1, Catherine E. Giguere-Rich, RD1, Gina N. Manzi, PharmD1, Donald Lum, MD, FACG3, Corey A. Siegel, MD, MS4
1Dartmouth-Hitchcock Medical Center, Lebanon, NH; 2Northwestern Medicine, Chicago, IL; 3The Oregon Clinic, Portland, OR; 4Dartmouth-Hitchcock Inflammatory Bowel Disease Center, Dartmouth-Hitchcock Medical Center, Lebanon, NH
Introduction: A goal of inflammatory bowel disease (IBD) management is to provide a multidisciplinary approach. Barriers include lack of resources outside of IBD centers and access to these specialty centers. Patients living in rural regions are particularly impacted by these barriers. Our aim was to create a comprehensive telehealth care model for patients living in rural regions called RADIUS (Rural Advanced Practice Providers Delivering IBD Care in the United States).
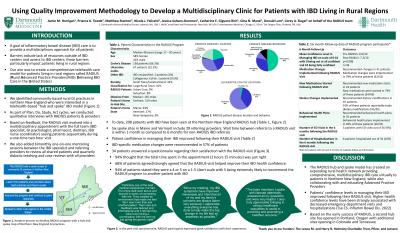
Methods: We identified community-based rural practices in northern New England who were interested in a telehealth-based “hub and spoke” IBD model (Figure 1). The initial iteration of a RADIUS visit included consultation with an IBD specialist and nurse coordinator and then optional visits later with an IBD psychologist, dietician, and pharmacist if deemed necessary. As part of Plan, Do, Study, Act (PDSA) cycles we conducted qualitative interviews with RADIUS patients and providers. Based on feedback, the next iteration included multidisciplinary appointments with the full team for all patients during a one-time two-hour virtual visit. We also added one-on-one mentoring sessions between the IBD specialist and referring providers on a bimonthly basis to review all shared patients and quarterly webinars providing didactic teaching and case reviews with all providers.
Results: To date, 161 patients (Table 1) with IBD have been seen at the Northern New England RADIUS hub. Six spoke sites in Maine and Vermont include 18 referring providers. Wait time between referral to a RADIUS visit is within 1 month as compared to 6 months for non-RADIUS IBD referrals. Average disease duration at time of referral has decreased from 32 years at RADIUS inception to 6 years currently. IBD-specific medication changes were made in 56% of patients. Qualitative referring provider and patient feedback was highly supportive of the new RADIUS care model.
Discussion: The RADIUS hub and spoke model has created an expanding rural health network providing comprehensive, multidisciplinary IBD care virtually to patients in Northern New England, while also collaborating with and educating Advanced Practice Providers. Using quality improvement methodology, we have co-developed a model with referring providers and patients to optimize the IBD care experience. Based on the early success of RADIUS, a second hub site has opened in Portland, Oregon with additional sites opening in 2023 in Colorado and Tennessee.

Disclosures:
Jamie M. Horrigan, MD1, Prianca K. Tawde, MD1, Matthew B. Stanton, MD2, Nicola J. Felicetti, RN1, Jessica Salwen-Deremer, PhD1, Catherine E. Giguere-Rich, RD1, Gina N. Manzi, PharmD1, Donald Lum, MD, FACG3, Corey A. Siegel, MD, MS4. P2123 - Using Quality Improvement Methodology to Develop a Multi-Disciplinary Clinic for Patients With IBD Living in Rural Regions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Dartmouth-Hitchcock Medical Center, Lebanon, NH; 2Northwestern Medicine, Chicago, IL; 3The Oregon Clinic, Portland, OR; 4Dartmouth-Hitchcock Inflammatory Bowel Disease Center, Dartmouth-Hitchcock Medical Center, Lebanon, NH
Introduction: A goal of inflammatory bowel disease (IBD) management is to provide a multidisciplinary approach. Barriers include lack of resources outside of IBD centers and access to these specialty centers. Patients living in rural regions are particularly impacted by these barriers. Our aim was to create a comprehensive telehealth care model for patients living in rural regions called RADIUS (Rural Advanced Practice Providers Delivering IBD Care in the United States).
Methods: We identified community-based rural practices in northern New England who were interested in a telehealth-based “hub and spoke” IBD model (Figure 1). The initial iteration of a RADIUS visit included consultation with an IBD specialist and nurse coordinator and then optional visits later with an IBD psychologist, dietician, and pharmacist if deemed necessary. As part of Plan, Do, Study, Act (PDSA) cycles we conducted qualitative interviews with RADIUS patients and providers. Based on feedback, the next iteration included multidisciplinary appointments with the full team for all patients during a one-time two-hour virtual visit. We also added one-on-one mentoring sessions between the IBD specialist and referring providers on a bimonthly basis to review all shared patients and quarterly webinars providing didactic teaching and case reviews with all providers.
Results: To date, 161 patients (Table 1) with IBD have been seen at the Northern New England RADIUS hub. Six spoke sites in Maine and Vermont include 18 referring providers. Wait time between referral to a RADIUS visit is within 1 month as compared to 6 months for non-RADIUS IBD referrals. Average disease duration at time of referral has decreased from 32 years at RADIUS inception to 6 years currently. IBD-specific medication changes were made in 56% of patients. Qualitative referring provider and patient feedback was highly supportive of the new RADIUS care model.
Discussion: The RADIUS hub and spoke model has created an expanding rural health network providing comprehensive, multidisciplinary IBD care virtually to patients in Northern New England, while also collaborating with and educating Advanced Practice Providers. Using quality improvement methodology, we have co-developed a model with referring providers and patients to optimize the IBD care experience. Based on the early success of RADIUS, a second hub site has opened in Portland, Oregon with additional sites opening in 2023 in Colorado and Tennessee.

Figure: Figure 1. Iterative process to develop RADIUS (Rural APPs Delivering IBD Care in the United States) program with hub and spoke map of Northern New England.
Disclosures:
Jamie Horrigan indicated no relevant financial relationships.
Prianca Tawde indicated no relevant financial relationships.
Matthew Stanton indicated no relevant financial relationships.
Nicola Felicetti indicated no relevant financial relationships.
Jessica Salwen-Deremer indicated no relevant financial relationships.
Catherine Giguere-Rich indicated no relevant financial relationships.
Gina Manzi indicated no relevant financial relationships.
Donald Lum: Abbvie – Speakers Bureau. Janssen – Speakers Bureau.
Corey Siegel: Abbvie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. BMS – Advisory Committee/Board Member, Consultant. Eli Lilly – Advisory Committee/Board Member, Consultant. Fresnius – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Consultant/advisory board, speaker for CME activities. Napo Pharmaceuticals – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau.
Jamie M. Horrigan, MD1, Prianca K. Tawde, MD1, Matthew B. Stanton, MD2, Nicola J. Felicetti, RN1, Jessica Salwen-Deremer, PhD1, Catherine E. Giguere-Rich, RD1, Gina N. Manzi, PharmD1, Donald Lum, MD, FACG3, Corey A. Siegel, MD, MS4. P2123 - Using Quality Improvement Methodology to Develop a Multi-Disciplinary Clinic for Patients With IBD Living in Rural Regions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
