Monday Poster Session
Category: IBD
P2125 - The Influence of End-Stage Renal Disease on Crohn’s Disease Hospitalizations: A Comparative Analysis in the United States
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- MZ
Mir Zulqarnain, DO
University of Missouri-Kansas City
Kansas City, MO
Presenting Author(s)
Vinay Jahagirdar, MD1, Mohamed Ahmed, MD1, Saqr Alsakarneh, MD1, Wael Mohamed, MD1, Mir Zulqarnain, DO1, Laith Al Momani, MD2, Hassan Ghoz, MD1, Francis A. Farraye, MD, MSc, MACG3
1University of Missouri-Kansas City, Kansas City, MO; 2Northwestern University, Chicago, IL; 3Mayo Clinic, Jacksonville, FL
Introduction: End-stage renal disease (ESRD), the final stage of chronic kidney disease (CKD) necessitating renal replacement therapy, is a growing public health problem placing major socio-economic burden on the health system. The incidence of ESRD in patients with Crohn’s disease (CD) is reported to be roughly 5 times higher than controls. This is attributed to systemic inflammation, autoimmune susceptibility, and metabolic and nutritional disorders due to chronic intestinal inflammation. We aim to look at outcomes of ESRD in patients with CD hospitalized in the US.
Methods: The National Inpatient Sample was used to identify all adult hospitalizations for patients with CD in the US between 2016-2020. The study population was divided into 2 groups based on the presence or absence of ESRD to compare hospitalization characteristics and outcomes. P-values < 0.05 were statistically significant.
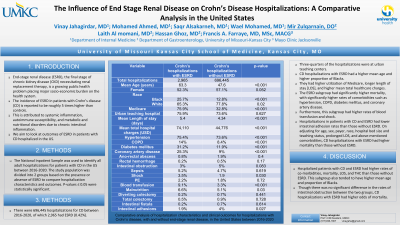
Results: There were 696,445 hospitalizations for CD between 2016-2020, of which 2,965 had ESRD (0.42%). Three-quarters of the hospitalizations were at urban teaching centers. CD hospitalizations with ESRD had a higher mean age (61.3 vs 47.6 years, p< 0.001). This subgroup also had a significantly higher proportion of Blacks (25.7% vs 12.8%, p< 0.001). They had higher utilization of Medicare (75.9% vs 32.8%, p< 0.001), longer length of stay [LOS] (5.39 vs 4.34 days, p< 0.001), and higher mean total healthcare charges (THC) ($74,110 vs $44,776, p< 0.001). The ESRD subgroup had significantly higher mortality (1.7% vs 0.2%, p< 0.001), with significantly higher rates of comorbidities such as hypertension, COPD, diabetes mellitus, and coronary artery disease. Furthermore, this subgroup had higher rates of blood transfusion (9.1% vs 3.3%, p< 0.001) and shock (3.5% vs 1.9%, p=0.03). Hospitalizations in patients with CD and ESRD had lower intestinal adhesion rates than those without ESRD (4% vs 1.9%, p=0.027). On adjusting for age, sex, payer, race, hospital bed size and teaching status, prolonged LOS, and above-mentioned comorbidities, CD hospitalizations with ESRD had higher mortality than those without ESRD (OR 5.42, 95% CI 2.23-9.17).
Discussion: Hospitalized patients with CD and ESRD had higher rates of co-morbidities, mortality, LOS, and THC than those without ESRD. This subgroup also tended to have higher mean age and proportion of Blacks. Though there was no significant difference in the rates of intestinal obstruction between the two groups, CD hospitalizations with ESRD had higher odds of mortality.

Disclosures:
Vinay Jahagirdar, MD1, Mohamed Ahmed, MD1, Saqr Alsakarneh, MD1, Wael Mohamed, MD1, Mir Zulqarnain, DO1, Laith Al Momani, MD2, Hassan Ghoz, MD1, Francis A. Farraye, MD, MSc, MACG3. P2125 - The Influence of End-Stage Renal Disease on Crohn’s Disease Hospitalizations: A Comparative Analysis in the United States, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Missouri-Kansas City, Kansas City, MO; 2Northwestern University, Chicago, IL; 3Mayo Clinic, Jacksonville, FL
Introduction: End-stage renal disease (ESRD), the final stage of chronic kidney disease (CKD) necessitating renal replacement therapy, is a growing public health problem placing major socio-economic burden on the health system. The incidence of ESRD in patients with Crohn’s disease (CD) is reported to be roughly 5 times higher than controls. This is attributed to systemic inflammation, autoimmune susceptibility, and metabolic and nutritional disorders due to chronic intestinal inflammation. We aim to look at outcomes of ESRD in patients with CD hospitalized in the US.
Methods: The National Inpatient Sample was used to identify all adult hospitalizations for patients with CD in the US between 2016-2020. The study population was divided into 2 groups based on the presence or absence of ESRD to compare hospitalization characteristics and outcomes. P-values < 0.05 were statistically significant.
Results: There were 696,445 hospitalizations for CD between 2016-2020, of which 2,965 had ESRD (0.42%). Three-quarters of the hospitalizations were at urban teaching centers. CD hospitalizations with ESRD had a higher mean age (61.3 vs 47.6 years, p< 0.001). This subgroup also had a significantly higher proportion of Blacks (25.7% vs 12.8%, p< 0.001). They had higher utilization of Medicare (75.9% vs 32.8%, p< 0.001), longer length of stay [LOS] (5.39 vs 4.34 days, p< 0.001), and higher mean total healthcare charges (THC) ($74,110 vs $44,776, p< 0.001). The ESRD subgroup had significantly higher mortality (1.7% vs 0.2%, p< 0.001), with significantly higher rates of comorbidities such as hypertension, COPD, diabetes mellitus, and coronary artery disease. Furthermore, this subgroup had higher rates of blood transfusion (9.1% vs 3.3%, p< 0.001) and shock (3.5% vs 1.9%, p=0.03). Hospitalizations in patients with CD and ESRD had lower intestinal adhesion rates than those without ESRD (4% vs 1.9%, p=0.027). On adjusting for age, sex, payer, race, hospital bed size and teaching status, prolonged LOS, and above-mentioned comorbidities, CD hospitalizations with ESRD had higher mortality than those without ESRD (OR 5.42, 95% CI 2.23-9.17).
Discussion: Hospitalized patients with CD and ESRD had higher rates of co-morbidities, mortality, LOS, and THC than those without ESRD. This subgroup also tended to have higher mean age and proportion of Blacks. Though there was no significant difference in the rates of intestinal obstruction between the two groups, CD hospitalizations with ESRD had higher odds of mortality.

Figure: Racial distribution for hospitalizations with Crohn’s disease, with and without end-stage renal disease in the United States from 2016-2020
Disclosures:
Vinay Jahagirdar indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Wael Mohamed indicated no relevant financial relationships.
Mir Zulqarnain indicated no relevant financial relationships.
Laith Al Momani indicated no relevant financial relationships.
Hassan Ghoz indicated no relevant financial relationships.
Francis Farraye: AbbVie – Advisory Committee/Board Member. Avalo Therapeutics – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. GSK – Advisory Committee/Board Member. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz Immunology – Advisory Committee/Board Member. Sebela – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Vinay Jahagirdar, MD1, Mohamed Ahmed, MD1, Saqr Alsakarneh, MD1, Wael Mohamed, MD1, Mir Zulqarnain, DO1, Laith Al Momani, MD2, Hassan Ghoz, MD1, Francis A. Farraye, MD, MSc, MACG3. P2125 - The Influence of End-Stage Renal Disease on Crohn’s Disease Hospitalizations: A Comparative Analysis in the United States, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
