Monday Poster Session
Category: IBD
P2133 - Prevalence and Predictors of Clostridioides difficile Infection Among Patients With Inflammatory Bowel Disease Who Have Undergone Bariatric Surgery
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Chidiebele E. Omaliko, MD
One Brooklyn Health-Brookdale University Hospital Medical Center
Brooklyn, NY
Presenting Author(s)
Chidiebele Omaliko, MD1, Rita Igwilo-Alaneme, MD2, Chimezie Mbachi, MD3, Chukwunonso B. Ezeani, MBBS4, Oghenefejiro Ogwor, MD5
1One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 2Montefiore Medical Center, Einstein Campus, Bronx, NY; 3Yale New Haven Hospital, New Haven, CT; 4Baton Rouge General Hospital, Baton Rouge, LA; 5St. Peters University Hospital, New Brunswick, NJ
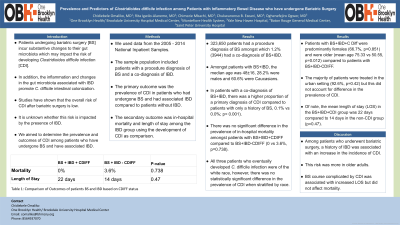
Introduction: Patients undergoing bariatric surgery [BS] incur substantive changes to their gut microbiota which may impact the risk of developing Clostridioides difficile infection [CDI]. In addition, the inflammation and changes in the gut microbiota associated with IBD promote C. difficile intestinal colonization. Studies have shown that the overall risk of CDI after bariatric surgery is low. It is unknown whether this risk is impacted by the presence of IBD. We aimed to determine the prevalence and outcomes of CDI among patients who have undergone BS and have associated IBD.
Methods: We used data from the 2005 - 2014 National Inpatient Samples. The sample population included patients with a procedure diagnosis of BS and a co-diagnosis of IBD. The primary outcome was the prevalence of CDI in patients who had undergone BS and had associated IBD compared to patients without IBD. The secondary outcome was in-hospital mortality and length of stay among in the IBD group using the development of CDI as comparison.
Results: 323,650 patients had a procedure diagnosis of BS amongst which 1.2% (3944) had a co-diagnosis of BS+IBD. Amongst patients with BS+IBD, the median age was 48±16, 28.2% were males and 60.6% were Caucasians. In patients with a co-diagnosis of BS+IBD, there was a higher proportion of a primary diagnosis of CDI compared to patients with only a history of BS, 0.1% vs 0.0%; p< 0.001). There was no significant difference in the prevalence of in-hospital mortality amongst patients with BS+IBD+CDIFF compared to BS+IBD-CDIFF (0 vs 3.6%, p=0.738). All three patients who eventually developed C. difficile infection were of the white race, however, there was no statistically significant difference in the prevalence of CDI when stratified by race. Patients with BS+IBD+C Diff were predominantly females (66.7%, p=0.851) and were older (mean age 75.33 vs 50.55, p=0.012) compared to patients with BS+IBD-CDIFF. The majority of patients were treated in the urban setting (92.6%, p=0.42) but this did not account for difference in the prevalence of CDI. Of note, the mean length of stay (LOS) in the BS+IBD+CDI group was 22 days compared to 14 days in the non-CDI group (p=0.47).
Discussion: Among patients who underwent bariatric surgery, a history of IBD was associated with an increase in the incidence of CDI. This risk was more in older adults. BS course complicated by CDI was associated with increased LOS but did not affect mortality.
Disclosures:
Chidiebele Omaliko, MD1, Rita Igwilo-Alaneme, MD2, Chimezie Mbachi, MD3, Chukwunonso B. Ezeani, MBBS4, Oghenefejiro Ogwor, MD5. P2133 - Prevalence and Predictors of Clostridioides difficile Infection Among Patients With Inflammatory Bowel Disease Who Have Undergone Bariatric Surgery, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 2Montefiore Medical Center, Einstein Campus, Bronx, NY; 3Yale New Haven Hospital, New Haven, CT; 4Baton Rouge General Hospital, Baton Rouge, LA; 5St. Peters University Hospital, New Brunswick, NJ
Introduction: Patients undergoing bariatric surgery [BS] incur substantive changes to their gut microbiota which may impact the risk of developing Clostridioides difficile infection [CDI]. In addition, the inflammation and changes in the gut microbiota associated with IBD promote C. difficile intestinal colonization. Studies have shown that the overall risk of CDI after bariatric surgery is low. It is unknown whether this risk is impacted by the presence of IBD. We aimed to determine the prevalence and outcomes of CDI among patients who have undergone BS and have associated IBD.
Methods: We used data from the 2005 - 2014 National Inpatient Samples. The sample population included patients with a procedure diagnosis of BS and a co-diagnosis of IBD. The primary outcome was the prevalence of CDI in patients who had undergone BS and had associated IBD compared to patients without IBD. The secondary outcome was in-hospital mortality and length of stay among in the IBD group using the development of CDI as comparison.
Results: 323,650 patients had a procedure diagnosis of BS amongst which 1.2% (3944) had a co-diagnosis of BS+IBD. Amongst patients with BS+IBD, the median age was 48±16, 28.2% were males and 60.6% were Caucasians. In patients with a co-diagnosis of BS+IBD, there was a higher proportion of a primary diagnosis of CDI compared to patients with only a history of BS, 0.1% vs 0.0%; p< 0.001). There was no significant difference in the prevalence of in-hospital mortality amongst patients with BS+IBD+CDIFF compared to BS+IBD-CDIFF (0 vs 3.6%, p=0.738). All three patients who eventually developed C. difficile infection were of the white race, however, there was no statistically significant difference in the prevalence of CDI when stratified by race. Patients with BS+IBD+C Diff were predominantly females (66.7%, p=0.851) and were older (mean age 75.33 vs 50.55, p=0.012) compared to patients with BS+IBD-CDIFF. The majority of patients were treated in the urban setting (92.6%, p=0.42) but this did not account for difference in the prevalence of CDI. Of note, the mean length of stay (LOS) in the BS+IBD+CDI group was 22 days compared to 14 days in the non-CDI group (p=0.47).
Discussion: Among patients who underwent bariatric surgery, a history of IBD was associated with an increase in the incidence of CDI. This risk was more in older adults. BS course complicated by CDI was associated with increased LOS but did not affect mortality.
Disclosures:
Chidiebele Omaliko indicated no relevant financial relationships.
Rita Igwilo-Alaneme indicated no relevant financial relationships.
Chimezie Mbachi indicated no relevant financial relationships.
Chukwunonso Ezeani indicated no relevant financial relationships.
Oghenefejiro Ogwor indicated no relevant financial relationships.
Chidiebele Omaliko, MD1, Rita Igwilo-Alaneme, MD2, Chimezie Mbachi, MD3, Chukwunonso B. Ezeani, MBBS4, Oghenefejiro Ogwor, MD5. P2133 - Prevalence and Predictors of Clostridioides difficile Infection Among Patients With Inflammatory Bowel Disease Who Have Undergone Bariatric Surgery, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
