Monday Poster Session
Category: IBD
P2137 - Validation of ICD-10-CM Diagnosis Codes in Patients With Inflammatory Bowel Disease in the National Veterans Affairs Healthcare System
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Paraj Patel, MD
Clement J. Zablocki VA Medical Center
Milwaukee, WI
Presenting Author(s)
Paraj Patel, MD1, Katherine Sherman, MS1, Saffia Bajwa, MD2, Julie Lorscheter, 1, Colleen Veenendaal, RN1, Mary Whooley, MD3, Katherine Hoggatt, PhD, MPH3, Salim Virani, MD, PhD4, Shirley Cohen-Mekelburg, MD, MS5, Emad Mansoor, MD6, Raymond K.. Cross, MD, MS, FACG7, Jeffrey Whittle, MD, MPH2, Jason Hou, MD, MS, FACG8, Preetika Sinh, MD2
1Clement J. Zablocki VA Medical Center, Milwaukee, WI; 2Medical College of Wisconsin, Milwaukee, WI; 3University of California San Francisco, San Francisco, CA; 4Aga Khan University, Karachi, Sindh, Pakistan; 5University of Michigan, Ann Arbor, MI; 6Case Western Reserve University / University Hospitals, Cleveland, OH; 7University of Maryland School of Medicine, Baltimore, MD; 8Baylor College of Medicine, Houston, TX
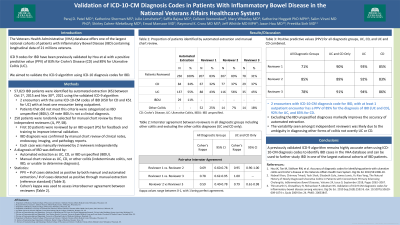
Introduction: We sought to determine if a previously validated algorithm for using International Classification of Diseases-9 (ICD-9) codes remained accurate when using ICD-10 codes to identify Inflammatory Bowel Diseases (IBD) [Ulcerative colitis (UC) and Crohn’s Disease (CD)] in the Veterans Health Administrative (VHA) database.
Methods: We identified IBD patients by automated data collection (ADC) between Oct 1, 2015 and Nov 30, 2021 from the VHA National Corporate Data Warehouse (CDW) by a previously validated ICD-9 algorithm [at least two VA encounters with an ICD-10 code for IBD (K51 UC or K50 CD) with at least one code from an outpatient encounter]. Cases that did not have the same IBD code on both encounters were classified as unspecified IBD (UIBD). Manual chart review (MCR) was performed by two independent reviewers (PP and LS) by review of clinical notes, endoscopy, imaging and pathology reports. Cases were categorized as IBD, UC, CD or other [indeterminate colitis (IC), unable to determine if IBD or not IBD]. The three data sets (ADC and 2 MCR) were assessed for concordance by Cohen’s kappa.
Results: We identified 57,823 IBD patients by ADC and randomly selected 250 patients, 134 UC (53.6%), 85 CD (34.0%) and 31 UIBD (12.4%) from VA facilities throughout the country for MCR. Reviewer 1 identified 104 (44.3%) as UC, 72 (30.6%) as CD, 3 (1.3%) as IC, 30 (12.8%) as unable to determine IBD diagnosis and 26 (11.1%) as not IBD. Reviewer 2 identified 99 (54.7%) as UC, 73 (40.3%) as CD, 1 (0.6%) as IC, 7 (3.9%) as unable to determine IBD diagnosis and 1 (0.6%) as not IBD. The algorithm had a positive predictive value (PPV) of 88.9 % to identify overall IBD diagnosis. The algorithm identified patients with CD and UC with high accuracy (concordance of 79.2% for CD and 94% for UC cases between reviewer 1 and ADC, 80.8% for CD and 95.6% for UC between reviewer 2 and ADC). After combining all IBD categories (UC, CD, other) the unweighted Cohen’s kappa between ADC and reviewer 1 (235 cases) was 0.501 (95% CI 0.418-0.584), between ADC and reviewer 2 (181 cases) was 0.735 (95% CI 0.650-0.820) and between reviewer 1 and reviewer 2 was 0.686 (95% CI 0.581-0.791).
Discussion: We validated an ICD-10 based algorithm to identify IBD cases in VHA datasets. It is highly accurate for UC (94%) and CD (80%) with an overall PPV of 88% for the diagnosis of IBD, similar to the ICD-9 based algorithm. Validation of ICD-10 IBD diagnosis codes is essential to study IBD in one of the largest national cohorts of IBD patients.
Disclosures:
Paraj Patel, MD1, Katherine Sherman, MS1, Saffia Bajwa, MD2, Julie Lorscheter, 1, Colleen Veenendaal, RN1, Mary Whooley, MD3, Katherine Hoggatt, PhD, MPH3, Salim Virani, MD, PhD4, Shirley Cohen-Mekelburg, MD, MS5, Emad Mansoor, MD6, Raymond K.. Cross, MD, MS, FACG7, Jeffrey Whittle, MD, MPH2, Jason Hou, MD, MS, FACG8, Preetika Sinh, MD2. P2137 - Validation of ICD-10-CM Diagnosis Codes in Patients With Inflammatory Bowel Disease in the National Veterans Affairs Healthcare System, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Clement J. Zablocki VA Medical Center, Milwaukee, WI; 2Medical College of Wisconsin, Milwaukee, WI; 3University of California San Francisco, San Francisco, CA; 4Aga Khan University, Karachi, Sindh, Pakistan; 5University of Michigan, Ann Arbor, MI; 6Case Western Reserve University / University Hospitals, Cleveland, OH; 7University of Maryland School of Medicine, Baltimore, MD; 8Baylor College of Medicine, Houston, TX
Introduction: We sought to determine if a previously validated algorithm for using International Classification of Diseases-9 (ICD-9) codes remained accurate when using ICD-10 codes to identify Inflammatory Bowel Diseases (IBD) [Ulcerative colitis (UC) and Crohn’s Disease (CD)] in the Veterans Health Administrative (VHA) database.
Methods: We identified IBD patients by automated data collection (ADC) between Oct 1, 2015 and Nov 30, 2021 from the VHA National Corporate Data Warehouse (CDW) by a previously validated ICD-9 algorithm [at least two VA encounters with an ICD-10 code for IBD (K51 UC or K50 CD) with at least one code from an outpatient encounter]. Cases that did not have the same IBD code on both encounters were classified as unspecified IBD (UIBD). Manual chart review (MCR) was performed by two independent reviewers (PP and LS) by review of clinical notes, endoscopy, imaging and pathology reports. Cases were categorized as IBD, UC, CD or other [indeterminate colitis (IC), unable to determine if IBD or not IBD]. The three data sets (ADC and 2 MCR) were assessed for concordance by Cohen’s kappa.
Results: We identified 57,823 IBD patients by ADC and randomly selected 250 patients, 134 UC (53.6%), 85 CD (34.0%) and 31 UIBD (12.4%) from VA facilities throughout the country for MCR. Reviewer 1 identified 104 (44.3%) as UC, 72 (30.6%) as CD, 3 (1.3%) as IC, 30 (12.8%) as unable to determine IBD diagnosis and 26 (11.1%) as not IBD. Reviewer 2 identified 99 (54.7%) as UC, 73 (40.3%) as CD, 1 (0.6%) as IC, 7 (3.9%) as unable to determine IBD diagnosis and 1 (0.6%) as not IBD. The algorithm had a positive predictive value (PPV) of 88.9 % to identify overall IBD diagnosis. The algorithm identified patients with CD and UC with high accuracy (concordance of 79.2% for CD and 94% for UC cases between reviewer 1 and ADC, 80.8% for CD and 95.6% for UC between reviewer 2 and ADC). After combining all IBD categories (UC, CD, other) the unweighted Cohen’s kappa between ADC and reviewer 1 (235 cases) was 0.501 (95% CI 0.418-0.584), between ADC and reviewer 2 (181 cases) was 0.735 (95% CI 0.650-0.820) and between reviewer 1 and reviewer 2 was 0.686 (95% CI 0.581-0.791).
Discussion: We validated an ICD-10 based algorithm to identify IBD cases in VHA datasets. It is highly accurate for UC (94%) and CD (80%) with an overall PPV of 88% for the diagnosis of IBD, similar to the ICD-9 based algorithm. Validation of ICD-10 IBD diagnosis codes is essential to study IBD in one of the largest national cohorts of IBD patients.
Disclosures:
Paraj Patel indicated no relevant financial relationships.
Katherine Sherman indicated no relevant financial relationships.
Saffia Bajwa indicated no relevant financial relationships.
Julie Lorscheter indicated no relevant financial relationships.
Colleen Veenendaal indicated no relevant financial relationships.
Mary Whooley indicated no relevant financial relationships.
Katherine Hoggatt indicated no relevant financial relationships.
Salim Virani: Abbvie – Consultant. Adiso – Consultant. BMS – Consultant. CorEvitas – Scientific Co-Director. Fresenius Kabi – Consultant. Fzata – Consultant. IBD Education Group – Member of Executive Committee. Janssen – Consultant. Janssen – Grant/Research Support. Pfizer – Consultant. Samsung Bioepis – Consultant. Sebela – Consultant. Takeda – Consultant.
Shirley Cohen-Mekelburg indicated no relevant financial relationships.
Emad Mansoor indicated no relevant financial relationships.
Raymond Cross: AbbVie – Consultant. Bristol Myers Squibb – Consultant. Janssen – Consultant. LabCorp – Consultant. Pfizer – Consultant. Samsung Bioepis – Consultant. Takeda – Consultant.
Jeffrey Whittle indicated no relevant financial relationships.
Jason Hou: Abbvie – Grant/Research Support. American Regent – Grant/Research Support. Celgene – Grant/Research Support. Pfizer – Grant/Research Support.
Preetika Sinh indicated no relevant financial relationships.
Paraj Patel, MD1, Katherine Sherman, MS1, Saffia Bajwa, MD2, Julie Lorscheter, 1, Colleen Veenendaal, RN1, Mary Whooley, MD3, Katherine Hoggatt, PhD, MPH3, Salim Virani, MD, PhD4, Shirley Cohen-Mekelburg, MD, MS5, Emad Mansoor, MD6, Raymond K.. Cross, MD, MS, FACG7, Jeffrey Whittle, MD, MPH2, Jason Hou, MD, MS, FACG8, Preetika Sinh, MD2. P2137 - Validation of ICD-10-CM Diagnosis Codes in Patients With Inflammatory Bowel Disease in the National Veterans Affairs Healthcare System, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
