Monday Poster Session
Category: IBD
P2141 - The Impact of Endoscopic Healing on Disease-Related Outcomes in Patients with Ulcerative Proctitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Esther Liu, BSc
Weill Cornell Medical College
New York, NY
Presenting Author(s)
Esther Liu, BSc1, Anjile An, MPH2, Robert Battat, MD3, Randy Longman, MD, PhD1, Ellen Scherl, MD, FACG4, Dana Lukin, MD, PhD, FACG4
1Weill Cornell Medical College, New York, NY; 2Weill Cornell Medicine, New York, NY; 3Centre hospitalier de l'Université de Montréal, Montreal, PQ, Canada; 4Jill Roberts Center for Inflammatory Bowel Disease, New York, NY
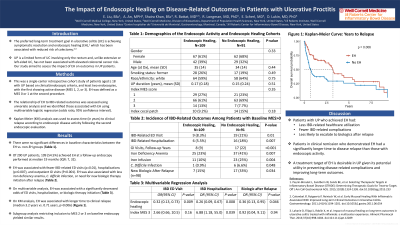
Introduction: The role of endoscopic healing (EH) in ulcerative proctitis (UP) is unclear. The long-term treatment goal in ulcerative colitis (UC) is achieving symptomatic resolution and EH, which has been associated with a reduced risk of colectomy. UP is a limited form of UC involving only the rectum and, unlike extensive/left-sided UC, has not been associated with elevated colorectal cancer risk. Therefore, achieving EH as compared to clinical remission in UP represents an uncertain therapeutic target.
Methods: This study assessed the impact of EH on outcomes in UP patients. This was a single-center, retrospective cohort study including patients aged ≥ 18 with a UP diagnosis based on clinical/endoscopic criteria. Patients had ≥2 endoscopies, with the first showing active disease (Mayo endoscopy score [(MES) of 1, 2, or 3]) and ≥1 month to the follow-up scope. EH was defined as an MES of 0 or 1 at the second scope. Descriptive statistics were used for baseline characteristics. The relationship of EH to IBD-related outcomes was assessed using univariate analysis (Pearson's Chi-squared test; Fisher's exact test; Welch Two Sample t-test) and those independently associated with EH were identified using logistic regression analysis (odds ratio, 95% confidence interval).
Results: Among 200 UP patients, 109 patients (54.5%) achieved EH. The median time from baseline to follow-up was 15 months (IQR: 6, 31). EH was associated with fewer IBD-related ED visits (EH: 8.3%, no EH: 21%) or hospitalizations (5.5% vs 18%) and fewer GI visits per follow-up year (mean: 1.47 [SD: 1.40], vs 2.96 [2.52]) after the follow-up scope. Patients with EH were less likely to have iron deficiency anemia (IDA; 23% vs 41%), iron infusion (10% vs 25%), C. difficile infection (0.9% vs 6.6%), or to initiate a new biologic after relapse (15% vs 33%). Patients with EH had a greater time to clinical relapse (650 days [730] vs 270 days [416]) (p=0.008). Patients with EH had reduced odds of an IBD-related ED visit (OR: 0.32, 95% CI: 0.13, 0.73) or hospitalization (0.26 [0.09, 0.67]), and 64% lower odds of biologic initiation after relapse (0.36 [0.13, 0.95]), adjusting for index MES score.
Discussion: UP patients with EH had less IBD-related healthcare utilization, fewer IBD-related complications, and were less likely to escalate to biologics after relapse than patients without EH. Using a treatment target of EH may be desirable in UP given its potential utility in preventing disease-related complications and improving long-term outcomes.
Disclosures:
Esther Liu, BSc1, Anjile An, MPH2, Robert Battat, MD3, Randy Longman, MD, PhD1, Ellen Scherl, MD, FACG4, Dana Lukin, MD, PhD, FACG4. P2141 - The Impact of Endoscopic Healing on Disease-Related Outcomes in Patients with Ulcerative Proctitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Weill Cornell Medical College, New York, NY; 2Weill Cornell Medicine, New York, NY; 3Centre hospitalier de l'Université de Montréal, Montreal, PQ, Canada; 4Jill Roberts Center for Inflammatory Bowel Disease, New York, NY
Introduction: The role of endoscopic healing (EH) in ulcerative proctitis (UP) is unclear. The long-term treatment goal in ulcerative colitis (UC) is achieving symptomatic resolution and EH, which has been associated with a reduced risk of colectomy. UP is a limited form of UC involving only the rectum and, unlike extensive/left-sided UC, has not been associated with elevated colorectal cancer risk. Therefore, achieving EH as compared to clinical remission in UP represents an uncertain therapeutic target.
Methods: This study assessed the impact of EH on outcomes in UP patients. This was a single-center, retrospective cohort study including patients aged ≥ 18 with a UP diagnosis based on clinical/endoscopic criteria. Patients had ≥2 endoscopies, with the first showing active disease (Mayo endoscopy score [(MES) of 1, 2, or 3]) and ≥1 month to the follow-up scope. EH was defined as an MES of 0 or 1 at the second scope. Descriptive statistics were used for baseline characteristics. The relationship of EH to IBD-related outcomes was assessed using univariate analysis (Pearson's Chi-squared test; Fisher's exact test; Welch Two Sample t-test) and those independently associated with EH were identified using logistic regression analysis (odds ratio, 95% confidence interval).
Results: Among 200 UP patients, 109 patients (54.5%) achieved EH. The median time from baseline to follow-up was 15 months (IQR: 6, 31). EH was associated with fewer IBD-related ED visits (EH: 8.3%, no EH: 21%) or hospitalizations (5.5% vs 18%) and fewer GI visits per follow-up year (mean: 1.47 [SD: 1.40], vs 2.96 [2.52]) after the follow-up scope. Patients with EH were less likely to have iron deficiency anemia (IDA; 23% vs 41%), iron infusion (10% vs 25%), C. difficile infection (0.9% vs 6.6%), or to initiate a new biologic after relapse (15% vs 33%). Patients with EH had a greater time to clinical relapse (650 days [730] vs 270 days [416]) (p=0.008). Patients with EH had reduced odds of an IBD-related ED visit (OR: 0.32, 95% CI: 0.13, 0.73) or hospitalization (0.26 [0.09, 0.67]), and 64% lower odds of biologic initiation after relapse (0.36 [0.13, 0.95]), adjusting for index MES score.
Discussion: UP patients with EH had less IBD-related healthcare utilization, fewer IBD-related complications, and were less likely to escalate to biologics after relapse than patients without EH. Using a treatment target of EH may be desirable in UP given its potential utility in preventing disease-related complications and improving long-term outcomes.
Disclosures:
Esther Liu indicated no relevant financial relationships.
Anjile An indicated no relevant financial relationships.
Robert Battat: Abbvie – Consultant. Bristol Myers Squibb – Consultant. Janssen – Consultant. Pfizer – Consultant. Prometheus – Consultant. Takeda – Consultant.
Randy Longman: enzymetrics – Consultant. Pfizer – Consultant.
Ellen Scherl: AbbVie – Consultant, Grant/Research Support. AstraZeneca – Grant/Research Support. Bristol Myers Squibb – Consultant. Celgen. R.B. – Grant/Research Support. Crohn’s and Colitis Foundation of America (CCFA) – Consultant, Grant/Research Support. Entera Health – Consultant. Evidera – Consultant, Grant/Research Support. Genentech – Grant/Research Support. GI Health Foundation – Consultant. Janssen – Consultant, Grant/Research Support. Johns Hopkins University – Grant/Research Support. National Institute of Diabetes and Digestive and Kidney (NIDDK) – Grant/Research Support. National Institute of Health (NIH) – Grant/Research Support. New York Crohn’s Foundation – Grant/Research Support. Pfizer – Grant/Research Support. Prometheus – Consultant. Protagonist Therapeutics – Consultant. Seres Health – Consultant. Seres Therapeutics – Grant/Research Support. Takeda Pharmaceuticals – Consultant. UCB – Grant/Research Support. UCSF–CCFA Clinical Research Alliance – Grant/Research Support.
Dana Lukin: Abbvie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol Myers Squibb – Advisory Committee/Board Member. Eli Lilly – Consultant. Fresenius Kabi – Consultant. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Magellan Health – Consultant. Palatin – Consultant. Pfizer – Consultant. Prometheus – Consultant. PSI – Consultant. Takeda – Consultant, Grant/Research Support.
Esther Liu, BSc1, Anjile An, MPH2, Robert Battat, MD3, Randy Longman, MD, PhD1, Ellen Scherl, MD, FACG4, Dana Lukin, MD, PhD, FACG4. P2141 - The Impact of Endoscopic Healing on Disease-Related Outcomes in Patients with Ulcerative Proctitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
