Monday Poster Session
Category: IBD
P2142 - Early Real-World Effectiveness and Safety of Upadacitinib in Crohn’s Disease: A Single-Center Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Esther Liu, BSc
Weill Cornell Medical College
New York, NY
Presenting Author(s)
Esther Liu, BSc1, Jordan Mandel, 2, Robert Battat, MD3, Randy Longman, MD, PhD1, Ellen Scherl, MD, FACG4, Dana Lukin, MD, PhD, FACG4
1Weill Cornell Medical College, New York, NY; 2Spence School, New York, NY; 3Centre hospitalier de l'Université de Montréal, Montreal, PQ, Canada; 4Jill Roberts Center for Inflammatory Bowel Disease, New York, NY
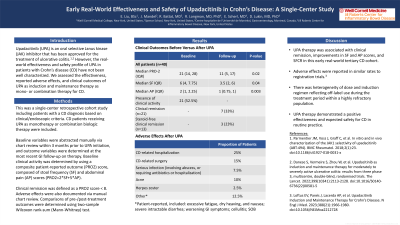
Introduction: The real-world effectiveness and safety of upadacitinib (UPA), an oral selective Janus kinase 1 inhibitor, in patients with Crohn’s disease (CD) have not been well characterized. We assessed the effectiveness, reported adverse effects, and clinical outcomes of UPA as induction and maintenance therapy as mono- or combination therapy for CD.
Methods: This was a single-center retrospective cohort study including patients with a CD diagnosis based on clinical/endoscopic criteria. CD patients receiving UPA as monotherapy or combination biologic therapy were included. Baseline variables were abstracted within 3 months prior to UPA initiation, and outcome variables were determined at the most recent GI follow-up on therapy. Baseline clinical activity was determined by using a composite patient-reported outcome (PRO2) score, composed of stool frequency (SF) and abdominal pain (AP) scores (PRO2=2*SF+5*AP). Clinical remission was defined as a PRO2 score < 8. Comparisons of pre-/post-treatment outcomes were determined using two-sample Wilcoxon rank-sum (Mann-Whitney) test.
Results: 40 CD patients receiving UPA were included; 28 (70%) were on UPA monotherapy, and 30% were on combination therapy. In the total cohort, 21 patients had baseline clinical activity; 33% achieved clinical remission. 19 patients did not have baseline activity (safety population). Prior to UPA, the median PRO-2 was 21 (IQR: 14, 28), decreasing to 11 (5, 17) after treatment (P=0.02). Median SF score was 6 (4, 7.75) before UPA, decreasing to 3.5 (2, 6) (P=0.04), and median AP score decreased from 2 (1, 2.25) to 1 (0.75, 1) (P=0.003). Of 13 patients with baseline activity and steroid use, 23% achieved steroid-free clinical remission (SFCR). While groups receiving mono-/combination therapy lacked sufficient size to detect differences in outcomes, numerical trends by subgroup were similar. 45% of patients on UPA reported an adverse event. 25% of patients reported a CD-related hospitalization, 15% underwent CD-related surgery, 7.5% reported a serious infection, 10% reported acne, and 2.5% reported herpes zoster.
Discussion: UPA therapy was associated with clinical remission, improvements in SF and AP scores, and SFCR in this early real-world tertiary CD cohort. Adverse effects were reported in similar rates to registration trials. There was heterogeneity of dose and induction regimen reflecting off-label use during the treatment period. UPA therapy demonstrated a positive efficacy and expected safety for CD in routine practice.
Disclosures:
Esther Liu, BSc1, Jordan Mandel, 2, Robert Battat, MD3, Randy Longman, MD, PhD1, Ellen Scherl, MD, FACG4, Dana Lukin, MD, PhD, FACG4. P2142 - Early Real-World Effectiveness and Safety of Upadacitinib in Crohn’s Disease: A Single-Center Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Weill Cornell Medical College, New York, NY; 2Spence School, New York, NY; 3Centre hospitalier de l'Université de Montréal, Montreal, PQ, Canada; 4Jill Roberts Center for Inflammatory Bowel Disease, New York, NY
Introduction: The real-world effectiveness and safety of upadacitinib (UPA), an oral selective Janus kinase 1 inhibitor, in patients with Crohn’s disease (CD) have not been well characterized. We assessed the effectiveness, reported adverse effects, and clinical outcomes of UPA as induction and maintenance therapy as mono- or combination therapy for CD.
Methods: This was a single-center retrospective cohort study including patients with a CD diagnosis based on clinical/endoscopic criteria. CD patients receiving UPA as monotherapy or combination biologic therapy were included. Baseline variables were abstracted within 3 months prior to UPA initiation, and outcome variables were determined at the most recent GI follow-up on therapy. Baseline clinical activity was determined by using a composite patient-reported outcome (PRO2) score, composed of stool frequency (SF) and abdominal pain (AP) scores (PRO2=2*SF+5*AP). Clinical remission was defined as a PRO2 score < 8. Comparisons of pre-/post-treatment outcomes were determined using two-sample Wilcoxon rank-sum (Mann-Whitney) test.
Results: 40 CD patients receiving UPA were included; 28 (70%) were on UPA monotherapy, and 30% were on combination therapy. In the total cohort, 21 patients had baseline clinical activity; 33% achieved clinical remission. 19 patients did not have baseline activity (safety population). Prior to UPA, the median PRO-2 was 21 (IQR: 14, 28), decreasing to 11 (5, 17) after treatment (P=0.02). Median SF score was 6 (4, 7.75) before UPA, decreasing to 3.5 (2, 6) (P=0.04), and median AP score decreased from 2 (1, 2.25) to 1 (0.75, 1) (P=0.003). Of 13 patients with baseline activity and steroid use, 23% achieved steroid-free clinical remission (SFCR). While groups receiving mono-/combination therapy lacked sufficient size to detect differences in outcomes, numerical trends by subgroup were similar. 45% of patients on UPA reported an adverse event. 25% of patients reported a CD-related hospitalization, 15% underwent CD-related surgery, 7.5% reported a serious infection, 10% reported acne, and 2.5% reported herpes zoster.
Discussion: UPA therapy was associated with clinical remission, improvements in SF and AP scores, and SFCR in this early real-world tertiary CD cohort. Adverse effects were reported in similar rates to registration trials. There was heterogeneity of dose and induction regimen reflecting off-label use during the treatment period. UPA therapy demonstrated a positive efficacy and expected safety for CD in routine practice.
Disclosures:
Esther Liu indicated no relevant financial relationships.
Jordan Mandel indicated no relevant financial relationships.
Robert Battat: Abbvie – Consultant. Bristol Myers Squibb – Consultant. Janssen – Consultant. Pfizer – Consultant. Prometheus – Consultant. Takeda – Consultant.
Randy Longman: enzymetrics – Consultant. Pfizer – Consultant.
Ellen Scherl: AbbVie – Consultant, Grant/Research Support. AstraZeneca – Grant/Research Support. Bristol Myers Squibb – Consultant. Celgen. R.B. – Grant/Research Support. Crohn’s and Colitis Foundation of America (CCFA) – Consultant, Grant/Research Support. Entera Health – Consultant. Evidera – Consultant, Grant/Research Support. Genentech – Grant/Research Support. GI Health Foundation – Consultant. Janssen – Consultant, Grant/Research Support. Johns Hopkins University – Grant/Research Support. National Institute of Diabetes and Digestive and Kidney (NIDDK) – Grant/Research Support. National Institute of Health (NIH) – Grant/Research Support. New York Crohn’s Foundation – Grant/Research Support. Pfizer – Grant/Research Support. Prometheus – Consultant. Protagonist Therapeutics – Consultant. Seres Health – Consultant. Seres Therapeutics – Grant/Research Support. Takeda Pharmaceuticals – Consultant. UCB – Grant/Research Support. UCSF–CCFA Clinical Research Alliance – Grant/Research Support.
Dana Lukin: Abbvie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol Myers Squibb – Advisory Committee/Board Member. Eli Lilly – Consultant. Fresenius Kabi – Consultant. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Magellan Health – Consultant. Palatin – Consultant. Pfizer – Consultant. Prometheus – Consultant. PSI – Consultant. Takeda – Consultant, Grant/Research Support.
Esther Liu, BSc1, Jordan Mandel, 2, Robert Battat, MD3, Randy Longman, MD, PhD1, Ellen Scherl, MD, FACG4, Dana Lukin, MD, PhD, FACG4. P2142 - Early Real-World Effectiveness and Safety of Upadacitinib in Crohn’s Disease: A Single-Center Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
