Monday Poster Session
Category: IBD
P2146 - No Impact of Primary Language on Treatment and Outcomes for Patients With Inflammatory Bowel Disease in Two Academic Medical Centers
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Veronica Chavez, MD
Dell Medical School at The University of Texas at Austin
Austin, Texas
Presenting Author(s)
Veronica Chavez, MD1, Jaya Vasudevan, MD1, Maria Goretti Ochi, MD1, Laura Sahyoun, MD2, Lawrence Kogan, MD2, Thritha Anand, 1, Jill Gaidos, MD, FACG2, Linda A. Feagins, MD, FACG1
1Dell Medical School at The University of Texas at Austin, Austin, TX; 2Yale University, New Haven, CT
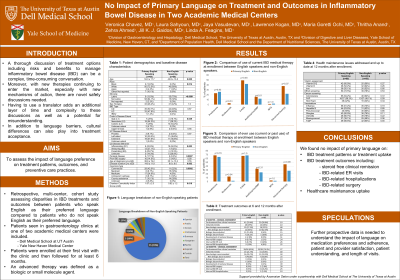
Introduction: A thorough discussion of treatment options to manage inflammatory bowel disease (IBD) can be a complex conversation. With many new therapies with new mechanisms of action there are novel safety discussions needed. Having to use a translator adds an additional layer of time and complexity to these discussions and potential for misunderstanding. We aimed to assess the impact of language preference on treatment patterns, outcomes, and preventive care practices.
Methods: A multi-center, retrospective, cohort study assessed IBD treatments and outcomes between patients who speak English as their preferred language (English group) compared to patients who do not speak English as their preferred language (non-English group). Patients seen in gastroenterology clinics at 1 of 2 academic medical centers were included. Patients were enrolled at their first clinic visit and then followed for ≥6 months. An advanced therapy was defined as a biologic or small molecule agent.
Results: We identified 119 patients with IBD (59 Crohn’s, 57 ulcerative colitis, 3 IBD undetermined) with 42% in the non-English group (70% Spanish). The non-English group were younger (53 vs 44, p=.005), more commonly white and Latino (70 vs 13%), had shorter disease duration (15 vs 9 years, p=.003), and less likely commercially insured (22 vs 42%, p=.0002). While no difference in rates of IBD type, the non-English group more commonly had colonic (20% vs 54%, p=.039) and inflammatory Crohn’s (23% vs 63%, p=.003), and were less likely to have perianal disease (17% vs 8%, p=.0007). There were no differences in baseline corticosteroid, advanced therapy, or narcotic use (Table). At 6 and 12 months, both groups had similar rates of steroid use or being recommended to start an advanced therapy. At 6 and 12 months, rates of IBD-related ER visits, hospitalizations, and surgery were not statistically different between the two groups. Preventive care practices were also similar between groups.
Discussion: In two IBD-focused academic practices where patients who don’t speak English are commonly seen, we found no impact of primary language on IBD treatment patterns, outcomes at 6 and 12 months including IBD-related ER visits, hospitalizations, and surgery, or preventive care practices. Further prospective data is needed to understand the impact of language on medication preferences and adherence, patient and provider satisfaction, patient understanding, and length of visits.
Disclosures:
Veronica Chavez, MD1, Jaya Vasudevan, MD1, Maria Goretti Ochi, MD1, Laura Sahyoun, MD2, Lawrence Kogan, MD2, Thritha Anand, 1, Jill Gaidos, MD, FACG2, Linda A. Feagins, MD, FACG1. P2146 - No Impact of Primary Language on Treatment and Outcomes for Patients With Inflammatory Bowel Disease in Two Academic Medical Centers, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Dell Medical School at The University of Texas at Austin, Austin, TX; 2Yale University, New Haven, CT
Introduction: A thorough discussion of treatment options to manage inflammatory bowel disease (IBD) can be a complex conversation. With many new therapies with new mechanisms of action there are novel safety discussions needed. Having to use a translator adds an additional layer of time and complexity to these discussions and potential for misunderstanding. We aimed to assess the impact of language preference on treatment patterns, outcomes, and preventive care practices.
Methods: A multi-center, retrospective, cohort study assessed IBD treatments and outcomes between patients who speak English as their preferred language (English group) compared to patients who do not speak English as their preferred language (non-English group). Patients seen in gastroenterology clinics at 1 of 2 academic medical centers were included. Patients were enrolled at their first clinic visit and then followed for ≥6 months. An advanced therapy was defined as a biologic or small molecule agent.
Results: We identified 119 patients with IBD (59 Crohn’s, 57 ulcerative colitis, 3 IBD undetermined) with 42% in the non-English group (70% Spanish). The non-English group were younger (53 vs 44, p=.005), more commonly white and Latino (70 vs 13%), had shorter disease duration (15 vs 9 years, p=.003), and less likely commercially insured (22 vs 42%, p=.0002). While no difference in rates of IBD type, the non-English group more commonly had colonic (20% vs 54%, p=.039) and inflammatory Crohn’s (23% vs 63%, p=.003), and were less likely to have perianal disease (17% vs 8%, p=.0007). There were no differences in baseline corticosteroid, advanced therapy, or narcotic use (Table). At 6 and 12 months, both groups had similar rates of steroid use or being recommended to start an advanced therapy. At 6 and 12 months, rates of IBD-related ER visits, hospitalizations, and surgery were not statistically different between the two groups. Preventive care practices were also similar between groups.
Discussion: In two IBD-focused academic practices where patients who don’t speak English are commonly seen, we found no impact of primary language on IBD treatment patterns, outcomes at 6 and 12 months including IBD-related ER visits, hospitalizations, and surgery, or preventive care practices. Further prospective data is needed to understand the impact of language on medication preferences and adherence, patient and provider satisfaction, patient understanding, and length of visits.
Disclosures:
Veronica Chavez indicated no relevant financial relationships.
Jaya Vasudevan indicated no relevant financial relationships.
Maria Goretti Ochi indicated no relevant financial relationships.
Laura Sahyoun indicated no relevant financial relationships.
Lawrence Kogan indicated no relevant financial relationships.
Thritha Anand indicated no relevant financial relationships.
Jill Gaidos: Abbvie – Advisor or Review Panel Member, Grant/Research Support. Bristol Myers Squibb – Grant/Research Support. Pfizer – Consultant, Grant/Research Support.
Linda A. Feagins: Bristol Myers Squibb – Grant/Research Support. Corevitas – Grant/Research Support. Takeda – Grant/Research Support.
Veronica Chavez, MD1, Jaya Vasudevan, MD1, Maria Goretti Ochi, MD1, Laura Sahyoun, MD2, Lawrence Kogan, MD2, Thritha Anand, 1, Jill Gaidos, MD, FACG2, Linda A. Feagins, MD, FACG1. P2146 - No Impact of Primary Language on Treatment and Outcomes for Patients With Inflammatory Bowel Disease in Two Academic Medical Centers, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

