Monday Poster Session
Category: IBD
P2162 - Variations in Score-Based Systems for the Evaluation of Remission and Treatment Response Among Patients With Ulcerative Colitis in Real-world Settings and Clinical Trials: A Pragmatic Review
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- AE
Alex Exuzides, PhD
Gilead
Foster City, California
Presenting Author(s)
Alex Exuzides, PhD1, Harry Jin, PhD, MPH2, Yan Zhong, PhD3, Emily Kaiser, BS4, Aaditya Rawal, MSc4, Shujun Gao, MBBS, PhD5, Barrett G. Levesque, MD, MS3
1Gilead, Foster City, CA; 2Gilead Sciences, Foster City, CA; 3Gilead Sciences, Inc., Foster City, CA; 4Costello Medical, Boston, MA; 5Gilead, Upper Saddle River, NJ
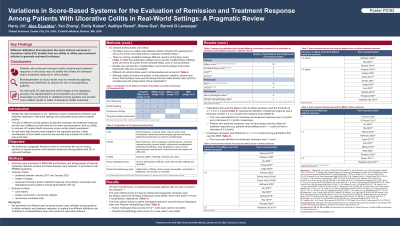
Introduction: Despite the high prevalence of ulcerative colitis (UC), there are multiple definitions used to characterize remission or measure treatment response. This limits the ability to apply these outcome measures to real-world evidence generation. We performed a pragmatic literature review to summarize the use of scoring systems to assess remission and treatment response among UC patients in real-world settings and randomized clinical trials (RCT).
Methods: Searches were conducted of MEDLINE, Embase, and bibliographies of all relevant publications in accordance with PRISMA guidelines. Inclusion criteria included studies published between Jan 2017–Jan 2023 that were written in English and measured remission and/or treatment response using clinical, endoscopic, and histologic scoring systems among adult UC patients. Exclusion criteria included studies that were case reports and studies conducted on non-human subjects.
Results: Of 3,821 records found, 33 studies of UC patients, including RCT and studies that analyzed real-world data, were included for this analysis. The Partial Mayo score and Mayo Endoscopic Score were the most utilized to measure clinical and endoscopic remission and were used in 21 and 16 studies, respectively (Table 1). The Nancy Histological Index and Robarts Histopathology Index were the most used histologic indices. Studies that used the Partial Mayo score to define remission either used the ≤1 or ≤2 point threshold, while the definition of treatment response was either a decrease of 2 or 3 points. In studies that used the Partial Mayo score, 31–61% of patients achieved remission in studies that used the ≤1 point definition compared to 19-81% in studies that used the ≤2 point definition. Similarly, studies that defined treatment response as a 2-point decrease reported a lower proportion of patients (19-64%) achieving treatment response compared to studies that used the 3-point decrease threshold (51-68%).
Discussion: Different definitions for clinical outcomes used across similar populations in UC studies decrease their utility to generate real-world data. Misinterpretation of study results may be avoided by applying standardized definitions to reduce the risk of misclassifying patients. As real-world UC data become more integral in the regulatory process, the standardization and consistent use of clinically meaningful cut points in validated scoring systems can provide more reliable results to better characterize health outcomes.
Disclosures:
Alex Exuzides, PhD1, Harry Jin, PhD, MPH2, Yan Zhong, PhD3, Emily Kaiser, BS4, Aaditya Rawal, MSc4, Shujun Gao, MBBS, PhD5, Barrett G. Levesque, MD, MS3. P2162 - Variations in Score-Based Systems for the Evaluation of Remission and Treatment Response Among Patients With Ulcerative Colitis in Real-world Settings and Clinical Trials: A Pragmatic Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Gilead, Foster City, CA; 2Gilead Sciences, Foster City, CA; 3Gilead Sciences, Inc., Foster City, CA; 4Costello Medical, Boston, MA; 5Gilead, Upper Saddle River, NJ
Introduction: Despite the high prevalence of ulcerative colitis (UC), there are multiple definitions used to characterize remission or measure treatment response. This limits the ability to apply these outcome measures to real-world evidence generation. We performed a pragmatic literature review to summarize the use of scoring systems to assess remission and treatment response among UC patients in real-world settings and randomized clinical trials (RCT).
Methods: Searches were conducted of MEDLINE, Embase, and bibliographies of all relevant publications in accordance with PRISMA guidelines. Inclusion criteria included studies published between Jan 2017–Jan 2023 that were written in English and measured remission and/or treatment response using clinical, endoscopic, and histologic scoring systems among adult UC patients. Exclusion criteria included studies that were case reports and studies conducted on non-human subjects.
Results: Of 3,821 records found, 33 studies of UC patients, including RCT and studies that analyzed real-world data, were included for this analysis. The Partial Mayo score and Mayo Endoscopic Score were the most utilized to measure clinical and endoscopic remission and were used in 21 and 16 studies, respectively (Table 1). The Nancy Histological Index and Robarts Histopathology Index were the most used histologic indices. Studies that used the Partial Mayo score to define remission either used the ≤1 or ≤2 point threshold, while the definition of treatment response was either a decrease of 2 or 3 points. In studies that used the Partial Mayo score, 31–61% of patients achieved remission in studies that used the ≤1 point definition compared to 19-81% in studies that used the ≤2 point definition. Similarly, studies that defined treatment response as a 2-point decrease reported a lower proportion of patients (19-64%) achieving treatment response compared to studies that used the 3-point decrease threshold (51-68%).
Discussion: Different definitions for clinical outcomes used across similar populations in UC studies decrease their utility to generate real-world data. Misinterpretation of study results may be avoided by applying standardized definitions to reduce the risk of misclassifying patients. As real-world UC data become more integral in the regulatory process, the standardization and consistent use of clinically meaningful cut points in validated scoring systems can provide more reliable results to better characterize health outcomes.
Disclosures:
Alex Exuzides indicated no relevant financial relationships.
Harry Jin indicated no relevant financial relationships.
Yan Zhong: Gilead Sciences – Employee, Stock Options.
Emily Kaiser: Costello Medical – Employee.
Aaditya Rawal: Costello Medical – Employee.
Shujun Gao: Gilead Sciences Inc – Employee.
Barrett Levesque: Gilead Sciences, Inc. – Employee.
Alex Exuzides, PhD1, Harry Jin, PhD, MPH2, Yan Zhong, PhD3, Emily Kaiser, BS4, Aaditya Rawal, MSc4, Shujun Gao, MBBS, PhD5, Barrett G. Levesque, MD, MS3. P2162 - Variations in Score-Based Systems for the Evaluation of Remission and Treatment Response Among Patients With Ulcerative Colitis in Real-world Settings and Clinical Trials: A Pragmatic Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
