Monday Poster Session
Category: IBD
P2170 - Candida Is Increased During Clinical Activity in Patients With Ulcerative Colitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Katie Hsia, MD
Tufts Medical Center
Boston, MA
Presenting Author(s)
Sushrut Jangi, MD1, Katie Hsia, MD1, Naisi Zhao, DrPH, MHS2, Carol Kumamoto, PhD2, Siddharth Singh, MD3, Sonia Friedman, MD2, Dominique Michaud, 2
1Tufts Medical Center, Boston, MA; 2Tufts University School of Medicine, Boston, MA; 3University of California, San Diego, San Diego, CA
Introduction: Gut microbial disruption has been implicated in the pathogenesis of ulcerative colitis (UC). There is increasing evidence that the fungal microbiome (mycobiome) may drive inflammation in mouse models of UC, and can prognosticate clinical response to fecal microbial transplantation among patients with UC. However, it remains unclear if fungal composition is altered during active compared to quiescent disease in UC.
Methods: We analyzed clinical and microbial sequencing data from the Study of a Prospective Adult Research Cohort with Inflammatory Bowel Disease. We evaluated the fungal composition of fecal samples from patients with UC during clinical activity and remission across varying severity indices. We assessed taxonomic changes cross-sectionally and dynamically over time. Additionally, we examined if there were shifts in specific amplicon sequence variants (ASVs) and fungal-bacterial correlations during activity and remission. Lastly, we examined if a random forest machine learning (RF) model (75% of the cohort for training, 25% for testing, with 10-fold cross-validation) using fungal taxonomic features could classify patients with activity or remission in UC.
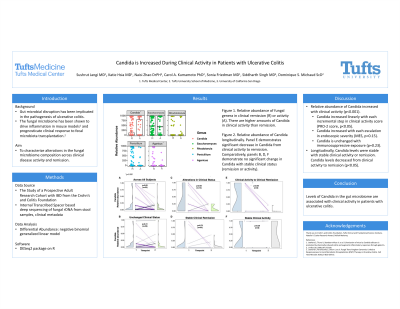
Results: There were 421 patients in our cohort, with 104 demonstrating clinical activity and 317 in remission. During clinical activity, the relative abundance (RA) of genus Candida was increased 3.5-fold (p-adj < 1 x 10-4) compared to during remission, adjusting for age, gender, and immunosuppressive exposure. Patients with changes in clinical status over time demonstrated alterations in Candida RA (p< 0.05), while longitudinal clinical stability was linked to stable Candida RA over time (p=0.32). We identified 5 unique Candida ASVs, with Candida albicans ASV RA associated with clinical activity. Candida RA correlated with relative abundance of bacterial taxa, including Parabacteroides diastonis (p< 0.05), Faecalibacterium prausnitzii (p< 0.05) and Bacteroides dorei (p< 0.05) during clinical remission, however these correlations were disrupted during activity. An RF model using the patient cohort could successfully classify patients as clinical active or quiescent (AUC=0.81), with Candida genus demonstrating strong feature importance.
Discussion: Clinical activity is associated with an increased relative abundance of Candida, cross-sectionally and dynamically, across a large UC patient cohort. Future studies may include trialing adjunctive antifungal treatments in patients with clinical activity to optimize disease outcomes.

Disclosures:
Sushrut Jangi, MD1, Katie Hsia, MD1, Naisi Zhao, DrPH, MHS2, Carol Kumamoto, PhD2, Siddharth Singh, MD3, Sonia Friedman, MD2, Dominique Michaud, 2. P2170 - Candida Is Increased During Clinical Activity in Patients With Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Tufts Medical Center, Boston, MA; 2Tufts University School of Medicine, Boston, MA; 3University of California, San Diego, San Diego, CA
Introduction: Gut microbial disruption has been implicated in the pathogenesis of ulcerative colitis (UC). There is increasing evidence that the fungal microbiome (mycobiome) may drive inflammation in mouse models of UC, and can prognosticate clinical response to fecal microbial transplantation among patients with UC. However, it remains unclear if fungal composition is altered during active compared to quiescent disease in UC.
Methods: We analyzed clinical and microbial sequencing data from the Study of a Prospective Adult Research Cohort with Inflammatory Bowel Disease. We evaluated the fungal composition of fecal samples from patients with UC during clinical activity and remission across varying severity indices. We assessed taxonomic changes cross-sectionally and dynamically over time. Additionally, we examined if there were shifts in specific amplicon sequence variants (ASVs) and fungal-bacterial correlations during activity and remission. Lastly, we examined if a random forest machine learning (RF) model (75% of the cohort for training, 25% for testing, with 10-fold cross-validation) using fungal taxonomic features could classify patients with activity or remission in UC.
Results: There were 421 patients in our cohort, with 104 demonstrating clinical activity and 317 in remission. During clinical activity, the relative abundance (RA) of genus Candida was increased 3.5-fold (p-adj < 1 x 10-4) compared to during remission, adjusting for age, gender, and immunosuppressive exposure. Patients with changes in clinical status over time demonstrated alterations in Candida RA (p< 0.05), while longitudinal clinical stability was linked to stable Candida RA over time (p=0.32). We identified 5 unique Candida ASVs, with Candida albicans ASV RA associated with clinical activity. Candida RA correlated with relative abundance of bacterial taxa, including Parabacteroides diastonis (p< 0.05), Faecalibacterium prausnitzii (p< 0.05) and Bacteroides dorei (p< 0.05) during clinical remission, however these correlations were disrupted during activity. An RF model using the patient cohort could successfully classify patients as clinical active or quiescent (AUC=0.81), with Candida genus demonstrating strong feature importance.
Discussion: Clinical activity is associated with an increased relative abundance of Candida, cross-sectionally and dynamically, across a large UC patient cohort. Future studies may include trialing adjunctive antifungal treatments in patients with clinical activity to optimize disease outcomes.

Figure: Candida relative abundance across disease activity. The panels demonstrate relative abundance of Candida over two time periods. Panel A includes all patients. Panel B includes patients with unchanged clinical status across the two time points. Panel C includes patients with changes in clinical status over the two time points. Panel D includes patients in stable clinical remission. Panel E includes patients who went from clinical activity to clinical remission. Panel F includes patients in stable clinical activity. There is a statistically significant change in relative abundance of candida in all subjects, driven by patients with alterations in clinical status (Panel C), particularly those with clinical activity to clinical remission (Panel E). Patients with stable amounts of activity or remission (B, D, F) did not have a statistically significant difference in Candida.
Disclosures:
Sushrut Jangi indicated no relevant financial relationships.
Katie Hsia indicated no relevant financial relationships.
Naisi Zhao indicated no relevant financial relationships.
Carol Kumamoto indicated no relevant financial relationships.
Siddharth Singh: Pfizer – Advisor or Review Panel Member, Grant/Research Support.
Sonia Friedman indicated no relevant financial relationships.
Dominique Michaud indicated no relevant financial relationships.
Sushrut Jangi, MD1, Katie Hsia, MD1, Naisi Zhao, DrPH, MHS2, Carol Kumamoto, PhD2, Siddharth Singh, MD3, Sonia Friedman, MD2, Dominique Michaud, 2. P2170 - Candida Is Increased During Clinical Activity in Patients With Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
