Monday Poster Session
Category: IBD
P2172 - Misdiagnosis of Inflammatory Bowel Disease: A Single-Center Case Series
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- RZ
Rasiq Zackria, DO
Sunrise Health Gastroenterology Fellowship
Las Vegas, Nevada
Presenting Author(s)
Rasiq Zackria, DO1, Robert Pattison, MD1, Youssef Ghobrial, MD2, Mark Hsu, MD3, Christian Diaz. Stone, MD4
1Sunrise Health Gastroenterology Fellowship, Las Vegas, NV; 2Sunrise Health GME Consortium, Las Vegas, NV; 3Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 4Inflammatory Bowel Disease Center, Comprehensive Digestive Institute of Nevada, Las Vegas, NV
Introduction: Inflammatory bowel disease (IBD), consisting of Crohn’s disease (CD) and ulcerative colitis (UC) may be challenging to diagnose. Because its presentation is often non-specific, numerous other intestinal conditions can mimic IBD, leading to misdiagnosis. In this retrospective, single-center study we investigated a series of patients misdiagnosed with IBD, aiming to describe the variables relating to the diagnostic error made.
Methods: The study population was derived from consecutive patients presenting to a gastroenterology community clinic between 2016-2021. Patients ≥18 years old were included if they presented with a prior established diagnosis of IBD, had received at least one IBD specific prescription medication, had all relevant prior medical records pertaining to the time of diagnosis, and were, based on our analysis, subsequently diagnosed with another non-IBD diagnosis. The prior IBD diagnosis was removed if clinical criteria for IBD were not sufficient to establish the diagnosis. We identified the errors that led to the IBD misdiagnosis (lack of chronic inflammation on pathology, misinterpretation of laboratory tests, and overreliance on serology testing). Descriptive statistics were used to analyze the data.
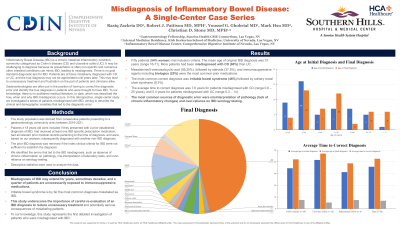
Results: 50 patients (54% women) met inclusion criteria. The mean age of original IBD diagnosis was 37 years (range 16-71). More patients had been misdiagnosed with CD (60%) than UC. Mesalamine/5-aminosalicyclic-acid (56.25%), followed by steroids (37.5%), and immunosuppressive agents including biologics (25%) were the most common prior medication. The most common correct diagnosis was irritable bowel syndrome (46%) followed by solitary rectal ulcer syndrome (9.3%). The average time to correct diagnosis was 7.6 years for patients misdiagnosed with CD (range 0.6–25 years), and 5.4 years for those misdiagnosed with UC (range 0.3–14). The most common sources of diagnostic error were misinterpretation of pathology and overreliance on IBD serology testing.
Discussion: Misdiagnosis of IBD may extend for years, sometimes decades, and a quarter of patients are unnecessarily exposed to immunosuppressive medications. Irritable bowel syndrome is by far the most common diagnosis mislabeled as IBD. This study underscores the importance of careful re-evaluation of an IBD diagnosis to reduce unnecessary treatment and potentially serious consequences of mislabeling patients. To our knowledge, this study represents the first detailed investigation of patients who were misdiagnosed with IBD.

Disclosures:
Rasiq Zackria, DO1, Robert Pattison, MD1, Youssef Ghobrial, MD2, Mark Hsu, MD3, Christian Diaz. Stone, MD4. P2172 - Misdiagnosis of Inflammatory Bowel Disease: A Single-Center Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Sunrise Health Gastroenterology Fellowship, Las Vegas, NV; 2Sunrise Health GME Consortium, Las Vegas, NV; 3Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 4Inflammatory Bowel Disease Center, Comprehensive Digestive Institute of Nevada, Las Vegas, NV
Introduction: Inflammatory bowel disease (IBD), consisting of Crohn’s disease (CD) and ulcerative colitis (UC) may be challenging to diagnose. Because its presentation is often non-specific, numerous other intestinal conditions can mimic IBD, leading to misdiagnosis. In this retrospective, single-center study we investigated a series of patients misdiagnosed with IBD, aiming to describe the variables relating to the diagnostic error made.
Methods: The study population was derived from consecutive patients presenting to a gastroenterology community clinic between 2016-2021. Patients ≥18 years old were included if they presented with a prior established diagnosis of IBD, had received at least one IBD specific prescription medication, had all relevant prior medical records pertaining to the time of diagnosis, and were, based on our analysis, subsequently diagnosed with another non-IBD diagnosis. The prior IBD diagnosis was removed if clinical criteria for IBD were not sufficient to establish the diagnosis. We identified the errors that led to the IBD misdiagnosis (lack of chronic inflammation on pathology, misinterpretation of laboratory tests, and overreliance on serology testing). Descriptive statistics were used to analyze the data.
Results: 50 patients (54% women) met inclusion criteria. The mean age of original IBD diagnosis was 37 years (range 16-71). More patients had been misdiagnosed with CD (60%) than UC. Mesalamine/5-aminosalicyclic-acid (56.25%), followed by steroids (37.5%), and immunosuppressive agents including biologics (25%) were the most common prior medication. The most common correct diagnosis was irritable bowel syndrome (46%) followed by solitary rectal ulcer syndrome (9.3%). The average time to correct diagnosis was 7.6 years for patients misdiagnosed with CD (range 0.6–25 years), and 5.4 years for those misdiagnosed with UC (range 0.3–14). The most common sources of diagnostic error were misinterpretation of pathology and overreliance on IBD serology testing.
Discussion: Misdiagnosis of IBD may extend for years, sometimes decades, and a quarter of patients are unnecessarily exposed to immunosuppressive medications. Irritable bowel syndrome is by far the most common diagnosis mislabeled as IBD. This study underscores the importance of careful re-evaluation of an IBD diagnosis to reduce unnecessary treatment and potentially serious consequences of mislabeling patients. To our knowledge, this study represents the first detailed investigation of patients who were misdiagnosed with IBD.

Figure: Pie chart demonstrating the final diagnosis of patient's misdiagnosed with IBD. The most common correct diagnosis was irritable bowel syndrome (46%) followed by solitary rectal ulcer syndrome (9.3%), NSAID-induced ulceration (3.7%) with the remaining 41% of cases comprising ten additional diagnoses.
Disclosures:
Rasiq Zackria indicated no relevant financial relationships.
Robert Pattison indicated no relevant financial relationships.
Youssef Ghobrial indicated no relevant financial relationships.
Mark Hsu indicated no relevant financial relationships.
Christian Stone: Abbvie – Speakers Bureau. Bristol Myers Squib – Speakers Bureau. Eli Lilly – Speakers Bureau. Janssen – Speakers Bureau. Pfizer – Speakers Bureau. Takeda – Speakers Bureau.
Rasiq Zackria, DO1, Robert Pattison, MD1, Youssef Ghobrial, MD2, Mark Hsu, MD3, Christian Diaz. Stone, MD4. P2172 - Misdiagnosis of Inflammatory Bowel Disease: A Single-Center Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
