Monday Poster Session
Category: IBD
P2176 - Healthcare Resource Utilization & Costs Across Different Sequences of Advanced Therapies in Patients With Crohn’s Disease or Ulcerative Colitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Tao Fan, MS, PhD
Takeda Pharmaceuticals U.S.A., Inc.
LEXINGTON, MA
Presenting Author(s)
Zaid Yousif, MS, PharmD, Tianming Zhang, PhD, Jeanne Jiang, PhD, Tao Fan, MS, PhD
Takeda Pharmaceuticals U.S.A., Inc., Lexington, MA
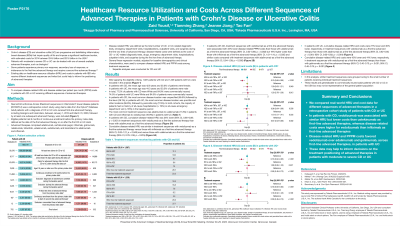
Introduction: Patients with moderate-to-severe inflammatory bowel disease (IBD) can be treated with one of several available advanced therapies and may receive a second-line therapy if the first treatment fails. Existing data on healthcare resource utilization (HRU) and costs in patients with IBD who receive different treatment sequences are limited.
Methods: Real wOrld ouTcomes Across tReatment sequences in inflammatorY bowel disease patients (ROTARY-2) was a retrospective cohort study using claims data from the Optum Database. Patients with Crohn’s disease (CD) or ulcerative colitis (UC) who received a first-line advanced therapy, including biologics and biosimilars, between January 1, 2013 and March 31, 2020, followed by at least one subsequent advanced therapy, were included. The effect of different treatment sequences on disease-related HRU and disease-related per patient per month (PPPM) costs across the treatment sequence was investigated using generalized linear regression models, adjusting for baseline demographics and clinical characteristics. Separate analyses were conducted for CD and UC.
Results: Overall, 1,587 patients with CD and 1,239 patients with UC met all eligibility criteria and were included in the analyses. In patients with CD, cumulative disease-related HRU was 24% lower for vedolizumab than adalimumab (p = 0.0002) as first-line advanced therapies but was similar for vedolizumab versus infliximab and versus ustekinumab. As first-line advanced therapies, vedolizumab had 33% lower disease-related PPPM costs than ustekinumab (p = 0.0016) and 19% higher costs than infliximab (p = 0.0350; Table 1). In patients with UC, cumulative disease-related HRU and PPPM costs were 27% lower and 30% lower, respectively, for vedolizumab than adalimumab (both p < 0.0001) and 42% lower and 41% lower, respectively, for vedolizumab than golimumab (both p < 0.0001) as first-line advanced therapies (Table 1).
Discussion: Disease-related HRU and PPPM costs varied among different treatment sequences, favoring vedolizumab over adalimumab and golimumab as first-line advanced therapies in patients with UC. In patients with CD, vedolizumab was associated with comparable HRU but lower costs than ustekinumab as first-line advanced therapies. These data may help to inform treatment decisions in patients with IBD.
Disclosures:
Zaid Yousif, MS, PharmD, Tianming Zhang, PhD, Jeanne Jiang, PhD, Tao Fan, MS, PhD. P2176 - Healthcare Resource Utilization & Costs Across Different Sequences of Advanced Therapies in Patients With Crohn’s Disease or Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Takeda Pharmaceuticals U.S.A., Inc., Lexington, MA
Introduction: Patients with moderate-to-severe inflammatory bowel disease (IBD) can be treated with one of several available advanced therapies and may receive a second-line therapy if the first treatment fails. Existing data on healthcare resource utilization (HRU) and costs in patients with IBD who receive different treatment sequences are limited.
Methods: Real wOrld ouTcomes Across tReatment sequences in inflammatorY bowel disease patients (ROTARY-2) was a retrospective cohort study using claims data from the Optum Database. Patients with Crohn’s disease (CD) or ulcerative colitis (UC) who received a first-line advanced therapy, including biologics and biosimilars, between January 1, 2013 and March 31, 2020, followed by at least one subsequent advanced therapy, were included. The effect of different treatment sequences on disease-related HRU and disease-related per patient per month (PPPM) costs across the treatment sequence was investigated using generalized linear regression models, adjusting for baseline demographics and clinical characteristics. Separate analyses were conducted for CD and UC.
Results: Overall, 1,587 patients with CD and 1,239 patients with UC met all eligibility criteria and were included in the analyses. In patients with CD, cumulative disease-related HRU was 24% lower for vedolizumab than adalimumab (p = 0.0002) as first-line advanced therapies but was similar for vedolizumab versus infliximab and versus ustekinumab. As first-line advanced therapies, vedolizumab had 33% lower disease-related PPPM costs than ustekinumab (p = 0.0016) and 19% higher costs than infliximab (p = 0.0350; Table 1). In patients with UC, cumulative disease-related HRU and PPPM costs were 27% lower and 30% lower, respectively, for vedolizumab than adalimumab (both p < 0.0001) and 42% lower and 41% lower, respectively, for vedolizumab than golimumab (both p < 0.0001) as first-line advanced therapies (Table 1).
Discussion: Disease-related HRU and PPPM costs varied among different treatment sequences, favoring vedolizumab over adalimumab and golimumab as first-line advanced therapies in patients with UC. In patients with CD, vedolizumab was associated with comparable HRU but lower costs than ustekinumab as first-line advanced therapies. These data may help to inform treatment decisions in patients with IBD.
Disclosures:
Zaid Yousif: Takeda Pharmaceuticals U.S.A., Inc – Consultant. University of California, San Diego – Assistant Clinical Professor.
Tianming Zhang: Takeda Pharmaceuticals U.S.A., Inc – Employee, Stock Options.
Jeanne Jiang: Takeda Pharmaceuticals U.S.A., Inc – Employee, Stock Options.
Tao Fan: Takeda Pharmaceuticals U.S.A., Inc – Employee, Stock Options.
Zaid Yousif, MS, PharmD, Tianming Zhang, PhD, Jeanne Jiang, PhD, Tao Fan, MS, PhD. P2176 - Healthcare Resource Utilization & Costs Across Different Sequences of Advanced Therapies in Patients With Crohn’s Disease or Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
