Monday Poster Session
Category: IBD
P2180 - In-Hospital Outcomes of Patients With Inflammatory Bowel Disease and Rheumatoid Arthritis: An Analysis of the National Inpatient Sample
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sajana Poudel, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL, IL
Presenting Author(s)
Sajana Poudel, MD1, Manoj Ghimire, MD2, Ayusha Poudel, MD3, Kalpana Ghimire, 4, Karun Shrestha, MD5, Prakriti Subedi, MD5, Calvin Ghimire, MD6, Sumina Rai, MBBS1, Muhammad Bilal Ibrahim, MD1, Rishab Khanal, MBBS7
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Mayo Clinic Florida, Jacksonville, FL; 3CCH, Chicago, IL; 4St. Barnabas Hospital, Bronx, NY; 5St. Barnabas Hospital, New York, NY; 6Michigan State University/McLaren Flint Hospital, Flint, MI; 7Sharada Metro Aspatal, Salyan, Rapti, Nepal
Introduction: Inflammatory bowel disease(IBD) includes ulcerative colitis and Crohn's disease characterized by relapsing and remitting episodes of inflammation in the intestine. Rheumatoid arthritis (RA) is a chronic autoimmune disease with both articular and extra-articular manifestations. Both RA and IBD are immune-mediated conditions that may arise from complex interactions between genetic and environmental factors. RA and IBD both being progressive and disabling disease, the co-occurrence of these two conditions, severely increases the disease burden and compromises the quality of life and prognosis of these patients.
Our objective was to compare the demographic and clinical characteristics, morality and inhosptial complications between two groups of study population.
Methods: All adult patients (age >18 years) with IBD with or without RA during hospital admission from 2016- 2020 were identified from the Nationwide Inpatient Sample. Data on demographic information, clinical characteristics, and outcome variables such as mortality, length of hospital stay, and hospital charges were analyzed using STATA v.17.
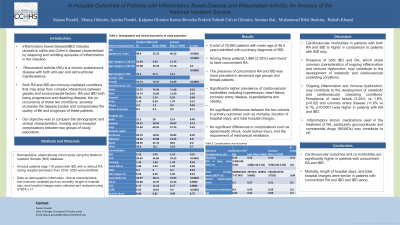
Results: A total of 79,060 patients with mean age of 46.5 years admitted with a primary diagnosis of IBD were included in the analysis. Among these patients,1,860 (2.35%) were found to have concomitant RA. The presence of concomitant RA and IBD was more prevalent in advanced age groups and female patients and had a significantly higher prevalence of cardiovascular morbidities including hypertension, heart failure, coronary artery disease, hyperlipidemia and obesity.
Our study did not find any significant differences between the two cohorts in primary outcomes such as mortality, duration of hospital stays, and total hospital charges. Additionally, complications such as sepsis/septic shock, acute kidney injury, and the requirement of mechanical ventilation were also similar between the two cohorts, The basic demographics and clinical characteristics of the study population is summarized in attached table.
Discussion: The prevalence of RA in patients with IBD in our study was 2.35% which is higher compared to the general population. Our study found significantly higher cardiovascular morbidities in patients with both RA and IBD in comparison to IBD only. It has been suggested that the presence of both IBD and RA, which share common characteristics of ongoing inflammation and immune dysfunction, may contribute to the development of metabolic and cardiovascular coexisting conditions.
Disclosures:
Sajana Poudel, MD1, Manoj Ghimire, MD2, Ayusha Poudel, MD3, Kalpana Ghimire, 4, Karun Shrestha, MD5, Prakriti Subedi, MD5, Calvin Ghimire, MD6, Sumina Rai, MBBS1, Muhammad Bilal Ibrahim, MD1, Rishab Khanal, MBBS7. P2180 - In-Hospital Outcomes of Patients With Inflammatory Bowel Disease and Rheumatoid Arthritis: An Analysis of the National Inpatient Sample, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Mayo Clinic Florida, Jacksonville, FL; 3CCH, Chicago, IL; 4St. Barnabas Hospital, Bronx, NY; 5St. Barnabas Hospital, New York, NY; 6Michigan State University/McLaren Flint Hospital, Flint, MI; 7Sharada Metro Aspatal, Salyan, Rapti, Nepal
Introduction: Inflammatory bowel disease(IBD) includes ulcerative colitis and Crohn's disease characterized by relapsing and remitting episodes of inflammation in the intestine. Rheumatoid arthritis (RA) is a chronic autoimmune disease with both articular and extra-articular manifestations. Both RA and IBD are immune-mediated conditions that may arise from complex interactions between genetic and environmental factors. RA and IBD both being progressive and disabling disease, the co-occurrence of these two conditions, severely increases the disease burden and compromises the quality of life and prognosis of these patients.
Our objective was to compare the demographic and clinical characteristics, morality and inhosptial complications between two groups of study population.
Methods: All adult patients (age >18 years) with IBD with or without RA during hospital admission from 2016- 2020 were identified from the Nationwide Inpatient Sample. Data on demographic information, clinical characteristics, and outcome variables such as mortality, length of hospital stay, and hospital charges were analyzed using STATA v.17.
Results: A total of 79,060 patients with mean age of 46.5 years admitted with a primary diagnosis of IBD were included in the analysis. Among these patients,1,860 (2.35%) were found to have concomitant RA. The presence of concomitant RA and IBD was more prevalent in advanced age groups and female patients and had a significantly higher prevalence of cardiovascular morbidities including hypertension, heart failure, coronary artery disease, hyperlipidemia and obesity.
Our study did not find any significant differences between the two cohorts in primary outcomes such as mortality, duration of hospital stays, and total hospital charges. Additionally, complications such as sepsis/septic shock, acute kidney injury, and the requirement of mechanical ventilation were also similar between the two cohorts, The basic demographics and clinical characteristics of the study population is summarized in attached table.
Discussion: The prevalence of RA in patients with IBD in our study was 2.35% which is higher compared to the general population. Our study found significantly higher cardiovascular morbidities in patients with both RA and IBD in comparison to IBD only. It has been suggested that the presence of both IBD and RA, which share common characteristics of ongoing inflammation and immune dysfunction, may contribute to the development of metabolic and cardiovascular coexisting conditions.
Disclosures:
Sajana Poudel indicated no relevant financial relationships.
Manoj Ghimire indicated no relevant financial relationships.
Ayusha Poudel indicated no relevant financial relationships.
Kalpana Ghimire indicated no relevant financial relationships.
Karun Shrestha indicated no relevant financial relationships.
Prakriti Subedi indicated no relevant financial relationships.
Calvin Ghimire indicated no relevant financial relationships.
Sumina Rai indicated no relevant financial relationships.
Muhammad Bilal Ibrahim indicated no relevant financial relationships.
Rishab Khanal indicated no relevant financial relationships.
Sajana Poudel, MD1, Manoj Ghimire, MD2, Ayusha Poudel, MD3, Kalpana Ghimire, 4, Karun Shrestha, MD5, Prakriti Subedi, MD5, Calvin Ghimire, MD6, Sumina Rai, MBBS1, Muhammad Bilal Ibrahim, MD1, Rishab Khanal, MBBS7. P2180 - In-Hospital Outcomes of Patients With Inflammatory Bowel Disease and Rheumatoid Arthritis: An Analysis of the National Inpatient Sample, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
