Monday Poster Session
Category: IBD
P2190 - The Association Between Ultra-Processed Food Consumption and Inflammatory Bowel Disease: A Meta-Analysis of Observational Studies
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- EH
Eric M. Hecht, MD, PhD
Institute of Etiological Research
Boca Raton, FL
Presenting Author(s)
Eric M. Hecht, MD, PhD1, David Landy, MD, PhD2, Deanna Ware, MPH3, Euridice Martinez, PhD4, Gary Adams, MD5
1Institute of Etiological Research, Boca Raton, FL; 2University of Kentucky, Lexinton, KY; 3Institute of Etiological Research, Washington, DC; 4University of Sao Paulo, Sao Paulo, Sao Paulo, Brazil; 5Prisma Health, Greenville, SC
Introduction: Inflammatory Bowel Disease (IBD) likely results from the interplay of genetic and environmental factors (including diet) that promote a proinflammatory intestinal milieu. The non-nutritional components of food including flavorings, colorings, emulsifiers, phosphates, maltodextrin, artificial sweeteners, carrageenan, carboxymethycellulose, polysorbate-80, aluminum, titanium dioxide, and other chemicals often found in processed/packaged food might also contribute to the development of IBD. Here we present the meta-analytic synthesis from several large, observational cohort studies in order to better understand the association between Ultra-processed food (UPF) consumption and IBD.
Methods: Article abstracts were located by searching PubMed using the combination of key terms Ultra-processed food AND Inflammatory Bowel Disease that were also the main variables of the study. Four longitudinal cohort studies were identified. We obtained the relative risk (RR) measure for IBD, Crohn’s disease and Ulcerative Colitis (UC) from each study. Several summary effect size measures were obtained by pooling the weighted individual study effect sizes using random effect modeling.
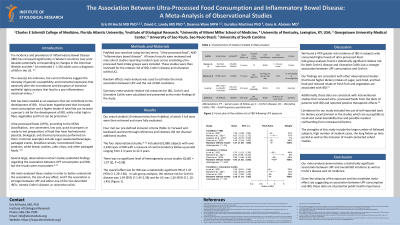
Results: Four of 10 relevant titles from PubMed, met our pre-defined inclusion criteria. The four observational studies included 652,880 subjects with over 2,240 cases of IBD with a follow-up period ranging from 2.3 to 22.3 years. The overall effect size for IBD was a statistically significant RR of 1.47 (95% CI 1.29-1.66). In sub-group analyses, the RR for Crohn’s disease was 1.94 (95% CI 1.45-2.58) and for UC was 1.26 (95% CI 1.10-1.45) (Figure 1)
Discussion: We found a 47% greater risk of IBD for individuals who consumed higher levels of UPF as compared to a reference group. Sub-group analyses found statistically significant elevated risks for both Crohn’s disease and UC. Our data are also consistent with other observational studies that found increased consumption of junk food, along with reduced intakes of fresh fruit and vegetables are associated with the development of IBD. Because Americans consume over 60% of their calories in the form of UPF reductions in this level of consumption could meaningfully decrease the incidence of IBD.

Disclosures:
Eric M. Hecht, MD, PhD1, David Landy, MD, PhD2, Deanna Ware, MPH3, Euridice Martinez, PhD4, Gary Adams, MD5. P2190 - The Association Between Ultra-Processed Food Consumption and Inflammatory Bowel Disease: A Meta-Analysis of Observational Studies, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Institute of Etiological Research, Boca Raton, FL; 2University of Kentucky, Lexinton, KY; 3Institute of Etiological Research, Washington, DC; 4University of Sao Paulo, Sao Paulo, Sao Paulo, Brazil; 5Prisma Health, Greenville, SC
Introduction: Inflammatory Bowel Disease (IBD) likely results from the interplay of genetic and environmental factors (including diet) that promote a proinflammatory intestinal milieu. The non-nutritional components of food including flavorings, colorings, emulsifiers, phosphates, maltodextrin, artificial sweeteners, carrageenan, carboxymethycellulose, polysorbate-80, aluminum, titanium dioxide, and other chemicals often found in processed/packaged food might also contribute to the development of IBD. Here we present the meta-analytic synthesis from several large, observational cohort studies in order to better understand the association between Ultra-processed food (UPF) consumption and IBD.
Methods: Article abstracts were located by searching PubMed using the combination of key terms Ultra-processed food AND Inflammatory Bowel Disease that were also the main variables of the study. Four longitudinal cohort studies were identified. We obtained the relative risk (RR) measure for IBD, Crohn’s disease and Ulcerative Colitis (UC) from each study. Several summary effect size measures were obtained by pooling the weighted individual study effect sizes using random effect modeling.
Results: Four of 10 relevant titles from PubMed, met our pre-defined inclusion criteria. The four observational studies included 652,880 subjects with over 2,240 cases of IBD with a follow-up period ranging from 2.3 to 22.3 years. The overall effect size for IBD was a statistically significant RR of 1.47 (95% CI 1.29-1.66). In sub-group analyses, the RR for Crohn’s disease was 1.94 (95% CI 1.45-2.58) and for UC was 1.26 (95% CI 1.10-1.45) (Figure 1)
Discussion: We found a 47% greater risk of IBD for individuals who consumed higher levels of UPF as compared to a reference group. Sub-group analyses found statistically significant elevated risks for both Crohn’s disease and UC. Our data are also consistent with other observational studies that found increased consumption of junk food, along with reduced intakes of fresh fruit and vegetables are associated with the development of IBD. Because Americans consume over 60% of their calories in the form of UPF reductions in this level of consumption could meaningfully decrease the incidence of IBD.

Figure: Forest plot demonstrating the relative risk of Inflammatory Bowel Disease following
exposure to ultra-processed foods
exposure to ultra-processed foods
Disclosures:
Eric Hecht indicated no relevant financial relationships.
David Landy indicated no relevant financial relationships.
Deanna Ware indicated no relevant financial relationships.
Euridice Martinez indicated no relevant financial relationships.
Gary Adams indicated no relevant financial relationships.
Eric M. Hecht, MD, PhD1, David Landy, MD, PhD2, Deanna Ware, MPH3, Euridice Martinez, PhD4, Gary Adams, MD5. P2190 - The Association Between Ultra-Processed Food Consumption and Inflammatory Bowel Disease: A Meta-Analysis of Observational Studies, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

