Monday Poster Session
Category: IBD
P2192 - Childhood Obesity Increases Risk of Adult-Onset IBD, but Adult-Onset Obesity May Lead to Worse Disease Outcomes
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Sara Kamionkowski, DO
MetroHealth Medical Center
Cleveland, OH
Presenting Author(s)
Sara Kamionkowski, DO1, Michael Kurin, MD2
1MetroHealth Medical Center, Cleveland, OH; 2MetroHealth, Cleveland, OH
Introduction: Inflammatory bowel disease (IBD) is often associated with malnutrition and weight loss, however the rate of obesity in IBD is upwards of 40%. Obesity in adulthood has been associated with worse outcomes in IBD, and studies have shown childhood obesity may increase the risk of Crohn’s disease as an adult, but not ulcerative colitis. But few studies assess the impact of childhood obesity on IBD disease severity. Our study aims to assess the impact of childhood obesity and adult-onset obesity on adult onset IBD.
Methods: A population-based retrospective analysis was performed using TriNetX, a global health research network. We compared IBD severity and outcomes for adult IBD patients who had childhood obesity (BMI >95 percentile) (C-OBESE), patients with adult-onset obesity (A-OBESE), and patients who never had obesity (NO-OBESE). We assessed surrogates for disease severity including pharmacotherapies, perianal disease, elevated fecal calprotectin (FCP) (≥120mcg/g), any bowel surgery, strictures, and hospitalization requiring intravenous (IV) steroids. One to one propensity score matching was performed for age, gender, race, tobacco use, and alcohol use. Risk of outcome for each comparison was described with adjusted odds ratio.
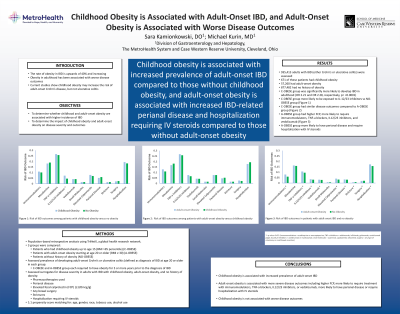
Results: About 935,413 adults had IBD of which 671 had childhood obesity, 57,260 had adult-onset obesity, and 877,482 never had any obesity. Those in the C-OBESE group were significantly more likely to develop Crohn’s disease or ulcerative colitis in adulthood (OR 2.21 and OR 2.28, respectively, p=< 0.001). Patients in the C-OBESE group were more likely to be exposed to IL-12/23 inhibitors versus those in the NO-OBESE group, but there were no other significant differences in medication exposures or clinical outcomes(Figure 1a). Those in the C-OBESE group had similar IBD outcomes compared to those in the A-OBESE group. (Figure1b). Patients in the A-OBESE group had higher FCP and were more likely to require treatment with immunomodulators, TNF-a blockers, IL12/IL23 inhibitors, and vedolizumab (Figure 1c). Patients in the A-OBESE group were more likely to have perianal disease and require hospitalization with IV steroids. IBD patients without obesity were more likely to have strictures or any type of surgery.
Discussion: Childhood obesity is associated with increased prevalence of adult-onset IBD. Unlike adult-onset obesity, which is associated with a more severe disease course, childhood obesity is not associated with worse disease outcomes in adult-onset IBD.

Disclosures:
Sara Kamionkowski, DO1, Michael Kurin, MD2. P2192 - Childhood Obesity Increases Risk of Adult-Onset IBD, but Adult-Onset Obesity May Lead to Worse Disease Outcomes, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1MetroHealth Medical Center, Cleveland, OH; 2MetroHealth, Cleveland, OH
Introduction: Inflammatory bowel disease (IBD) is often associated with malnutrition and weight loss, however the rate of obesity in IBD is upwards of 40%. Obesity in adulthood has been associated with worse outcomes in IBD, and studies have shown childhood obesity may increase the risk of Crohn’s disease as an adult, but not ulcerative colitis. But few studies assess the impact of childhood obesity on IBD disease severity. Our study aims to assess the impact of childhood obesity and adult-onset obesity on adult onset IBD.
Methods: A population-based retrospective analysis was performed using TriNetX, a global health research network. We compared IBD severity and outcomes for adult IBD patients who had childhood obesity (BMI >95 percentile) (C-OBESE), patients with adult-onset obesity (A-OBESE), and patients who never had obesity (NO-OBESE). We assessed surrogates for disease severity including pharmacotherapies, perianal disease, elevated fecal calprotectin (FCP) (≥120mcg/g), any bowel surgery, strictures, and hospitalization requiring intravenous (IV) steroids. One to one propensity score matching was performed for age, gender, race, tobacco use, and alcohol use. Risk of outcome for each comparison was described with adjusted odds ratio.
Results: About 935,413 adults had IBD of which 671 had childhood obesity, 57,260 had adult-onset obesity, and 877,482 never had any obesity. Those in the C-OBESE group were significantly more likely to develop Crohn’s disease or ulcerative colitis in adulthood (OR 2.21 and OR 2.28, respectively, p=< 0.001). Patients in the C-OBESE group were more likely to be exposed to IL-12/23 inhibitors versus those in the NO-OBESE group, but there were no other significant differences in medication exposures or clinical outcomes(Figure 1a). Those in the C-OBESE group had similar IBD outcomes compared to those in the A-OBESE group. (Figure1b). Patients in the A-OBESE group had higher FCP and were more likely to require treatment with immunomodulators, TNF-a blockers, IL12/IL23 inhibitors, and vedolizumab (Figure 1c). Patients in the A-OBESE group were more likely to have perianal disease and require hospitalization with IV steroids. IBD patients without obesity were more likely to have strictures or any type of surgery.
Discussion: Childhood obesity is associated with increased prevalence of adult-onset IBD. Unlike adult-onset obesity, which is associated with a more severe disease course, childhood obesity is not associated with worse disease outcomes in adult-onset IBD.

Figure: Figure 1: Risk of IBD outcomes among patients with childhood obesity versus no obesity (A). Risk of IBD outcomes among patients with adult-onset obesity versus childhood obesity (B). Risk of IBD outcomes in patients with adult-onset IBD and no obesity (C). * = p value <0.05. (Immunomodulators = azathioprine or mercaptopurine; TNF-a inhibitors = adalimumab, infliximab, golimumab, certolizumab pegol; IL12/IL23 inhibitors = ustekinumab or risankizumab; small molecules = ozanimod, upadacitinib, tofacitinib; surgery = any type of colectomy or small bowel resection)
Disclosures:
Sara Kamionkowski indicated no relevant financial relationships.
Michael Kurin indicated no relevant financial relationships.
Sara Kamionkowski, DO1, Michael Kurin, MD2. P2192 - Childhood Obesity Increases Risk of Adult-Onset IBD, but Adult-Onset Obesity May Lead to Worse Disease Outcomes, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
