Monday Poster Session
Category: IBD
P2211 - Hepatic Impact of Etrasimod for Treatment of Moderately to Severely Active Ulcerative Colitis: An Integrated Safety Summary From the Etrasimod Ulcerative Colitis Clinical Program
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Miguel Regueiro, MD
Cleveland Clinic Lerner College of Medicine, Case Western Reserve University
Cleveland, Ohio
Presenting Author(s)
Miguel Regueiro, MD1, Séverine Vermeire, MD, PhD2, David T. Rubin, MD3, Marla C. Dubinsky, MD4, Ailsa Hart, BMBCh, PhD5, Joseph Wu, PhD6, Jesse Green, MD7, John C.. Woolcott, PhD7, Kenneth J.. Gorelick, MD7, Aoibhinn McDonnell, PhD8, Krisztina Lazin, MD9, Laurent Peyrin-Biroulet, MD, PhD10
1Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH; 2UZ Leuven, Leuven, Vlaams-Brabant, Belgium; 3Inflammatory Bowel Disease Center, University of Chicago Medicine, Chicago, IL; 4Mount Sinai Kravis Children’s Hospital, New York, NY; 5St. Mark’s Hospital & Imperial College, London, England, United Kingdom; 6Pfizer Inc., Cambridge, MA; 7Pfizer Inc., Collegeville, PA; 8Pfizer Ltd., Sandwich, England, United Kingdom; 9Pfizer AG, Zurich, Zurich, Switzerland; 10Last Inserm U954 and CHU de Nancy, Lorraine University, Vandoeuvre-lès-Nancy, Lorraine, France
Introduction: Etrasimod is an investigational, oral, once-daily, selective sphingosine 1-phosphate (S1P)1,4,5 receptor modulator in development for the treatment of moderately to severely active ulcerative colitis (UC). Patients (pts) with inflammatory bowel disease may experience changes in liver function tests,1 with liver adverse events (AEs) reported in previous S1P receptor modulator trials.2
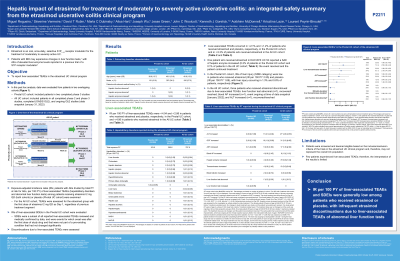
Methods: Here, we report liver-associated treatment-emergent AEs (TEAEs) from the etrasimod UC clinical program. Pts in the phase (p)2 (OASIS, NCT02447302), p3 (ELEVATE UC 52, NCT03945188; ELEVATE UC 12, NCT03996369), and p2 and p3 open-label extension (OLE) studies (NCT02536404; NCT03950232; NCT04176588 [data snapshot January 31, 2022]) were evaluated in two data cohorts: Pivotal UC (ELEVATE UC 52 and ELEVATE 12) and All UC (all p2, p3, and OLE studies). Exposure-adjusted incidence rates (EAIRs; number of pts with AEs divided by total pt-years [PY] at risk for AEs), of liver-related TEAEs, per 1 PY for hepatobiliary disorders and per 100 PY for investigations among pts receiving etrasimod (2 mg once daily, both cohorts) or placebo (PBO; Pivotal UC cohort) were examined. EAIRs, per 100 PY, of liver-related sponsor-designated events of interest (SDEIs) in the Pivotal UC cohort, and discontinuations due to liver-related TEAEs in the All UC cohort, were assessed.
Results: In the Pivotal UC cohort (etrasimod, N=527; PBO, N=260), incidence of liver-related TEAEs was higher in etrasimod- (EAIR ≤ 4.04) vs PBO-treated (EAIRs ≤ 2.86) pts (Table). Similarly, in the All UC cohort (etrasimod, N=942), EAIRs of liver-related TEAEs were ≤ 4.06 (Table). Proportions of pts with liver-related TEAEs across both cohorts were ≤ 3.3% and ≤ 1.2% for etrasimod- and PBO-treated pts, respectively. In the Pivotal UC cohort, incidence of SDEIs in etrasimod- (EAIR ≤ 2.55) and PBO-treated (EAIR ≤ 1.89) pts was low, and occurred in 1.3% and 0.8% of pts, respectively (Table). In the All UC cohort, three etrasimod-treated pts discontinued due to liver-related TEAEs: abnormal liver function test, increased blood alkaline phosphatase, and increased alanine aminotransferase, respectively.
Discussion: Incidence of liver-related TEAEs and SDEIs was generally low among pts treated with etrasimod and PBO with infrequent etrasimod discontinuations due to liver-related TEAEs.
References:
1. Harbord M et al. J Crohns Colitis 2016; 10: 239–254.
2. Sandborn WJ et al. N Engl J Med 2021; 285: 1280–1291.
Disclosures:
Miguel Regueiro, MD1, Séverine Vermeire, MD, PhD2, David T. Rubin, MD3, Marla C. Dubinsky, MD4, Ailsa Hart, BMBCh, PhD5, Joseph Wu, PhD6, Jesse Green, MD7, John C.. Woolcott, PhD7, Kenneth J.. Gorelick, MD7, Aoibhinn McDonnell, PhD8, Krisztina Lazin, MD9, Laurent Peyrin-Biroulet, MD, PhD10. P2211 - Hepatic Impact of Etrasimod for Treatment of Moderately to Severely Active Ulcerative Colitis: An Integrated Safety Summary From the Etrasimod Ulcerative Colitis Clinical Program, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH; 2UZ Leuven, Leuven, Vlaams-Brabant, Belgium; 3Inflammatory Bowel Disease Center, University of Chicago Medicine, Chicago, IL; 4Mount Sinai Kravis Children’s Hospital, New York, NY; 5St. Mark’s Hospital & Imperial College, London, England, United Kingdom; 6Pfizer Inc., Cambridge, MA; 7Pfizer Inc., Collegeville, PA; 8Pfizer Ltd., Sandwich, England, United Kingdom; 9Pfizer AG, Zurich, Zurich, Switzerland; 10Last Inserm U954 and CHU de Nancy, Lorraine University, Vandoeuvre-lès-Nancy, Lorraine, France
Introduction: Etrasimod is an investigational, oral, once-daily, selective sphingosine 1-phosphate (S1P)1,4,5 receptor modulator in development for the treatment of moderately to severely active ulcerative colitis (UC). Patients (pts) with inflammatory bowel disease may experience changes in liver function tests,1 with liver adverse events (AEs) reported in previous S1P receptor modulator trials.2
Methods: Here, we report liver-associated treatment-emergent AEs (TEAEs) from the etrasimod UC clinical program. Pts in the phase (p)2 (OASIS, NCT02447302), p3 (ELEVATE UC 52, NCT03945188; ELEVATE UC 12, NCT03996369), and p2 and p3 open-label extension (OLE) studies (NCT02536404; NCT03950232; NCT04176588 [data snapshot January 31, 2022]) were evaluated in two data cohorts: Pivotal UC (ELEVATE UC 52 and ELEVATE 12) and All UC (all p2, p3, and OLE studies). Exposure-adjusted incidence rates (EAIRs; number of pts with AEs divided by total pt-years [PY] at risk for AEs), of liver-related TEAEs, per 1 PY for hepatobiliary disorders and per 100 PY for investigations among pts receiving etrasimod (2 mg once daily, both cohorts) or placebo (PBO; Pivotal UC cohort) were examined. EAIRs, per 100 PY, of liver-related sponsor-designated events of interest (SDEIs) in the Pivotal UC cohort, and discontinuations due to liver-related TEAEs in the All UC cohort, were assessed.
Results: In the Pivotal UC cohort (etrasimod, N=527; PBO, N=260), incidence of liver-related TEAEs was higher in etrasimod- (EAIR ≤ 4.04) vs PBO-treated (EAIRs ≤ 2.86) pts (Table). Similarly, in the All UC cohort (etrasimod, N=942), EAIRs of liver-related TEAEs were ≤ 4.06 (Table). Proportions of pts with liver-related TEAEs across both cohorts were ≤ 3.3% and ≤ 1.2% for etrasimod- and PBO-treated pts, respectively. In the Pivotal UC cohort, incidence of SDEIs in etrasimod- (EAIR ≤ 2.55) and PBO-treated (EAIR ≤ 1.89) pts was low, and occurred in 1.3% and 0.8% of pts, respectively (Table). In the All UC cohort, three etrasimod-treated pts discontinued due to liver-related TEAEs: abnormal liver function test, increased blood alkaline phosphatase, and increased alanine aminotransferase, respectively.
Discussion: Incidence of liver-related TEAEs and SDEIs was generally low among pts treated with etrasimod and PBO with infrequent etrasimod discontinuations due to liver-related TEAEs.
References:
1. Harbord M et al. J Crohns Colitis 2016; 10: 239–254.
2. Sandborn WJ et al. N Engl J Med 2021; 285: 1280–1291.
Disclosures:
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Alfasigma – Advisory Committee/Board Member, Consultant. Allergan – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Celgene – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Eli Lilly – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Gilead Sciences – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Janssen – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Miraca Labs – Advisory Committee/Board Member, Consultant. Pfizer Inc – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Seres – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Target RWE – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant, Unrestricted educational grants. Wolters Kluwer Health – Royalties.
Séverine Vermeire: AbbVie – Consultant, Grant/Research Support. AbolerIS Pharma – Grant/Research Support. AgomAb – Grant/Research Support. Alimentiv – Consultant. Arena Pharmaceuticals – Consultant. AstraZeneca – Consultant. Avaxia Biologics – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Celgene – Consultant. CVasThera – Consultant, Speakers Bureau. Cytoki Pharma – Consultant, Speakers Bureau. Dr. Falk Pharma – Consultant, Speakers Bureau. Eli Lilly – Consultant, Speakers Bureau. Ferring Pharmaceuticals – Consultant, Speakers Bureau. Galapagos – Consultant, Grant/Research Support, Speakers Bureau. Genentech/Roche – Consultant, Speakers Bureau. Gilead – Consultant, Speakers Bureau. GSK – Consultant, Speakers Bureau. Hospira – Consultant, Speakers Bureau. IMIDomics – Consultant, Speakers Bureau. Janssen Pharmaceuticals – Consultant, Speakers Bureau. Johnson & Johnson – Consultant, Grant/Research Support, Speakers Bureau. Materia Prima – Consultant, Speakers Bureau. MiroBio – Consultant, Speakers Bureau. Morphic – Consultant, Speakers Bureau. MRM Health – Consultant, Speakers Bureau. MSD – Consultant, Speakers Bureau. Mundipharma – Consultant, Speakers Bureau. Pfizer – Consultant, Grant/Research Support, Speakers Bureau. ProDigest – Consultant, Speakers Bureau. Progenity – Consultant, Speakers Bureau. Prometheus – Consultant, Speakers Bureau. Robarts Clinical Trials – Consultant, Speakers Bureau. Second Genome – Consultant, Speakers Bureau. Shire – Consultant, Speakers Bureau. Surrozen – Consultant, Speakers Bureau. Takeda – Consultant, Grant/Research Support, Speakers Bureau. Theravance Biopharma – Consultant, Speakers Bureau. Tillotts Pharma – Consultant, Speakers Bureau. Zealand Pharma – Consultant, Speakers Bureau.
David Rubin: AbbVie – Consultant, personal fees. AltruBio – Consultant, personal fees. Aslan Pharmaceuticals – Consultant. Athos Therapeutics – Consultant. Bellatrix Pharmaceuticals – Consultant. Boehringer Ingelheim – Consultant, personal fees. Bristol Myers Squibb – Consultant. Celgene Chronicles – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Corp/Syneos – Consultant. Eco R1 – Consultant. GastroIntestinal Research Foundation – Grant/Research Support. Genentech/Roche – Consultant. Gilead Sciences – Consultant, personal fees. Helmsley Charitable Trust – Grant/Research Support. Iterative Health – Consultant. Janssen Pharmaceuticals – Consultant, personal fees. Kaleido Biosciences – Consultant. Lilly – Consultant. Pfizer – Consultant, personal fees. Prometheus Biosciences – Consultant. Reistone Biopharma – Consultant, personal fees. Seres Therapeutics – Consultant. Takeda – Consultant, Grant/Research Support, Personal fees. Target RWE – Consultant. Trellus Health – Consultant.
Marla Dubinsky: AbbVie – Consultant, Grant/Research Support. Arena Pharmaceuticals – Consultant. Astra Zeneca – Consultant. Celgene – Consultant. Genentech Inc. – Consultant. Gilead Sciences – Consultant. Janssen – Consultant, Grant/Research Support. Merck – Consultant. Pfizer – Consultant, Grant/Research Support. Prometheus Biosciences – Consultant, Grant/Research Support. Prometheus Labs – Consultant, Grant/Research Support. Takeda – Consultant, Licensing fees. Thabor – Consultant. Trellus Health – Stock-publicly held company(excluding mutual/index funds). UCB Pharma – Consultant.
Ailsa Hart: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau. Atlantic Pharmaceuticals – Advisory Committee/Board Member, Consultant, Speakers Bureau. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speakers Bureau. Celltrion – Advisory Committee/Board Member, Consultant, Speakers Bureau. Falk – Advisory Committee/Board Member, Consultant, Speakers Bureau. Ferring – Advisory Committee/Board Member, Consultant, Speakers Bureau. Genentech – Global Steering Committee. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. MSD – Advisory Committee/Board Member, Consultant, Speakers Bureau. Napp Pharmaceuticals – Advisory Committee/Board Member, Consultant, Speakers Bureau. Pfizer – Advisory Committee/Board Member, Consultant, Speakers Bureau. Pharmacosmos – Advisory Committee/Board Member, Consultant, Speakers Bureau. Shire – Advisory Committee/Board Member, Consultant, Speakers Bureau. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Joseph Wu: Pfizer Inc – Employee, Stock Options.
Jesse Green: Pfizer Inc – Employee, Stock-publicly held company(excluding mutual/index funds).
John Woolcott: Pfizer Inc – Employee, Stock Options.
Kenneth Gorelick: Arena – Consultant. Pfizer Inc – Consultant. Zymo Consulting Group – Independent Contractor.
Aoibhinn McDonnell: Pfizer Ltd – Employee, Stock Options.
Krisztina Lazin: Pfizer AG – Employee, Stock Options.
Laurent Peyrin-Biroulet: AbbVie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Allergan – personal fees. Alma – personal fees. Amgen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Applied Molecular Transport – personal fees. Arena – personal fees. Biogaran – Advisory Committee/Board Member, Consultant, Speakers Bureau. Biogen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant, Speakers Bureau. Bristol Myers Squibb – personal fees. Celgene – Advisory Committee/Board Member, Consultant, Speakers Bureau. Celltrion – Advisory Committee/Board Member, Consultant, Speakers Bureau. CTMA – Stock Options. Eli Lilly – Advisory Committee/Board Member, Consultant, Speakers Bureau. Enterome – personal fees. Enthera – personal fees. Ferring – Advisory Committee/Board Member, Consultant, Speakers Bureau. Forward Pharma – Advisory Committee/Board Member, Consultant, Speakers Bureau. Fresenius – personal fees. Genentech – Advisory Committee/Board Member, Consultant, Speakers Bureau. Gilead – personal fees. H.A.C. Pharma – Advisory Committee/Board Member, Consultant, Speakers Bureau. Hikma – personal fees. Hospira/Pfizer – Advisory Committee/Board Member, Consultant, Speakers Bureau. Index Pharmaceuticals – Advisory Committee/Board Member, Consultant, Speakers Bureau. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Lycera – Advisory Committee/Board Member, Consultant, Speakers Bureau. Merck – Advisory Committee/Board Member, Consultant, Speakers Bureau. Mitsubishi – Advisory Committee/Board Member, Consultant, Speakers Bureau. MSD – Grant/Research Support, personal fees. Mylan – personal fees. Nestlé – personal fees. Norgine – Advisory Committee/Board Member, Consultant, Speakers Bureau. Oppilan Pharma – personal fees. OSE Immunotherapeutics – personal fees. Pfizer – personal fees. Pharmacosmos – personal fees. Roche – personal fees. Samsung Bioepis – Advisory Committee/Board Member, Consultant, Speakers Bureau. Sandoz – Advisory Committee/Board Member, Consultant, Speakers Bureau. Sterna – personal fees. Sublimity Therapeutics – personal fees. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau. Theravance – Advisory Committee/Board Member, Consultant, Speakers Bureau. Tillots – Advisory Committee/Board Member, Consultant, Speakers Bureau. Vifor – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Miguel Regueiro, MD1, Séverine Vermeire, MD, PhD2, David T. Rubin, MD3, Marla C. Dubinsky, MD4, Ailsa Hart, BMBCh, PhD5, Joseph Wu, PhD6, Jesse Green, MD7, John C.. Woolcott, PhD7, Kenneth J.. Gorelick, MD7, Aoibhinn McDonnell, PhD8, Krisztina Lazin, MD9, Laurent Peyrin-Biroulet, MD, PhD10. P2211 - Hepatic Impact of Etrasimod for Treatment of Moderately to Severely Active Ulcerative Colitis: An Integrated Safety Summary From the Etrasimod Ulcerative Colitis Clinical Program, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
