Monday Poster Session
Category: IBD
P2219 - Lower Substance Use, but Higher Opioid Use, Among Hospitalizations with Inflammatory Bowel Disease: National Inpatient Sample
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- JK
Jin Sun Kim, MD
Keck School of Medicine of USC
Los Angeles, CA
Presenting Author(s)
Jin Sun Kim, MD1, Patrick Chang, MD2, Jason Hung, MS2, Sarah Sheibani, MD2, Florence-Damilola Odufalu, MD2, Cynthia Cherfane, MD2, Jennifer L. Dodge, MPH2, Bing Zhang, MD2
1Keck School of Medicine of USC, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: Inflammatory Bowel Disease (IBD) is associated with chronic pain and increased psychosocial burden. While the connection of substance use disorder (SUD) among IBD patients has been theorized, the epidemiology has not been thoroughly investigated. We aim to compare the prevalence of overall and substance-specific SUD in hospitalizations with and without IBD.
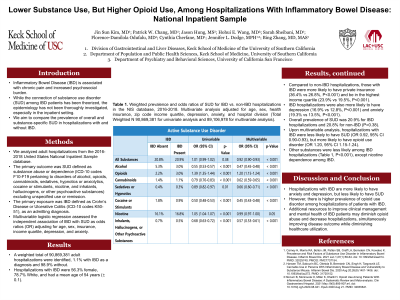
Methods: We analyzed adult hospitalizations from the 2016-2018 United States National Inpatient Sample database. The primary outcome was SUD defined as substance abuse or dependence (ICD-10 codes F10-F19 pertaining to disorders of alcohol, opioids, cannabinoids, sedatives, hypnotics or anxiolytics, cocaine or stimulants, nicotine, and inhalants, hallucinogens, or other psychoactive substances) excluding unspecified use or remission. The primary exposure was IBD defined as Crohn’s Disease or Ulcerative Colitis (ICD-10 codes K50-51), as an admitting diagnosis. Multivariable logistic regression assessed the independent association of IBD with SUD as odds ratios (OR) adjusting for age, sex, insurance, income quartile, depression, and anxiety.
Results: A weighted total of 90,869,381 adult hospitalizations were identified, 1.1% with IBD as a diagnosis and 98.9% without. Hospitalizations with IBD were 56.3% female, 78.7% White, and had a mean age of 54 years (± 0.1). Compared to non-IBD hospitalizations, those with IBD were more likely to have private insurance (36.4% vs 26.8%, P< 0.001) and be in the 4th income quartile (23.9% vs 19.5%, P< 0.001). IBD hospitalizations were also more likely to have depression (16.9% vs 12.8%, P< 0.001) and anxiety (19.3% vs 13.5%, P< 0.001). Overall prevalence of SUD was 20.9% for IBD hospitalizations and 20.8% for non-IBD (P=0.38). Upon multivariable analysis, hospitalizations with IBD were less likely to have SUD (OR 0.93, 95% CI 0.91-0.94), but more likely to have opioid use disorder (OR 1.22, 95% CI 1.18-1.26). Other substances were less likely among IBD hospitalizations (Table 1, P< 0.001), but we did not detect a significant difference in nicotine dependence by IBD.
Discussion: Hospitalizations with IBD are more likely to have anxiety and depression, but less likely to have SUD. This study highlights the increased prevalence of opioid use disorder in hospitalizations with IBD. Careful assessment of specific substances supports the need for further interventions to reduce opioid abuse in IBD, especially given unfavorable IBD-related consequences and the opioid epidemic.
Disclosures:
Jin Sun Kim, MD1, Patrick Chang, MD2, Jason Hung, MS2, Sarah Sheibani, MD2, Florence-Damilola Odufalu, MD2, Cynthia Cherfane, MD2, Jennifer L. Dodge, MPH2, Bing Zhang, MD2. P2219 - Lower Substance Use, but Higher Opioid Use, Among Hospitalizations with Inflammatory Bowel Disease: National Inpatient Sample, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Keck School of Medicine of USC, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: Inflammatory Bowel Disease (IBD) is associated with chronic pain and increased psychosocial burden. While the connection of substance use disorder (SUD) among IBD patients has been theorized, the epidemiology has not been thoroughly investigated. We aim to compare the prevalence of overall and substance-specific SUD in hospitalizations with and without IBD.
Methods: We analyzed adult hospitalizations from the 2016-2018 United States National Inpatient Sample database. The primary outcome was SUD defined as substance abuse or dependence (ICD-10 codes F10-F19 pertaining to disorders of alcohol, opioids, cannabinoids, sedatives, hypnotics or anxiolytics, cocaine or stimulants, nicotine, and inhalants, hallucinogens, or other psychoactive substances) excluding unspecified use or remission. The primary exposure was IBD defined as Crohn’s Disease or Ulcerative Colitis (ICD-10 codes K50-51), as an admitting diagnosis. Multivariable logistic regression assessed the independent association of IBD with SUD as odds ratios (OR) adjusting for age, sex, insurance, income quartile, depression, and anxiety.
Results: A weighted total of 90,869,381 adult hospitalizations were identified, 1.1% with IBD as a diagnosis and 98.9% without. Hospitalizations with IBD were 56.3% female, 78.7% White, and had a mean age of 54 years (± 0.1). Compared to non-IBD hospitalizations, those with IBD were more likely to have private insurance (36.4% vs 26.8%, P< 0.001) and be in the 4th income quartile (23.9% vs 19.5%, P< 0.001). IBD hospitalizations were also more likely to have depression (16.9% vs 12.8%, P< 0.001) and anxiety (19.3% vs 13.5%, P< 0.001). Overall prevalence of SUD was 20.9% for IBD hospitalizations and 20.8% for non-IBD (P=0.38). Upon multivariable analysis, hospitalizations with IBD were less likely to have SUD (OR 0.93, 95% CI 0.91-0.94), but more likely to have opioid use disorder (OR 1.22, 95% CI 1.18-1.26). Other substances were less likely among IBD hospitalizations (Table 1, P< 0.001), but we did not detect a significant difference in nicotine dependence by IBD.
Discussion: Hospitalizations with IBD are more likely to have anxiety and depression, but less likely to have SUD. This study highlights the increased prevalence of opioid use disorder in hospitalizations with IBD. Careful assessment of specific substances supports the need for further interventions to reduce opioid abuse in IBD, especially given unfavorable IBD-related consequences and the opioid epidemic.
Disclosures:
Jin Sun Kim indicated no relevant financial relationships.
Patrick Chang indicated no relevant financial relationships.
Jason Hung indicated no relevant financial relationships.
Sarah Sheibani indicated no relevant financial relationships.
Florence-Damilola Odufalu indicated no relevant financial relationships.
Cynthia Cherfane indicated no relevant financial relationships.
Jennifer Dodge indicated no relevant financial relationships.
Bing Zhang indicated no relevant financial relationships.
Jin Sun Kim, MD1, Patrick Chang, MD2, Jason Hung, MS2, Sarah Sheibani, MD2, Florence-Damilola Odufalu, MD2, Cynthia Cherfane, MD2, Jennifer L. Dodge, MPH2, Bing Zhang, MD2. P2219 - Lower Substance Use, but Higher Opioid Use, Among Hospitalizations with Inflammatory Bowel Disease: National Inpatient Sample, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
