Monday Poster Session
Category: IBD
P2227 - Longitudinal Trends in Inflammatory Bowel Disease Hospitalizations in the Era of Biologics: A 20 Year Nationwide Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Ellen J. Spartz, MD
UCLA
Los Angeles, CA
Presenting Author(s)
Ellen J. Spartz, MD, Vivy Cusumano, MD, Jenny Sauk, MD, Berkeley Limketkai, MD, PhD
UCLA, Los Angeles, CA
Introduction: Infliximab was the first biologic approved for Crohn’s disease (CD) in 1998, heralding an era of powerful immunosuppressive therapies. Two decades later, there are 11 FDA-approved biologic agents and small molecule inhibitors for the management of inflammatory bowel disease (IBD). It remains unclear whether the availability of these agents has had an impact on hospitalizations, a surrogate for IBD disease severity and failure of outpatient medical treatments. The aim of this study was to examine the overall epidemiology and longitudinal trends of IBD-related hospitalizations in the era of biologics.
Methods: This retrospective study analyzed the National Inpatient Sample (NIS) databases from 1998-2018. Hospitalizations for ulcerative colitis (UC) and CD were identified by the International Classification of Diseases (ICD)-9 and 10 codes in the first 3 diagnosis positions. Hospitalization trends were evaluated according to time, age group (every 2 decades), sex, and race. Denominators included IBD-only hospitalizations, all-cause hospitalizations, and the United States (US) population.
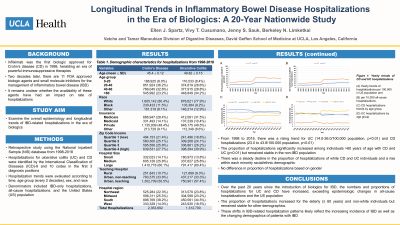
Results: From 1998 through 2018, there was a rising trend for UC (14.0 to 26.0/100,000 population; p trend< 0.01) and CD hospitalizations (23.0 to 43.8/100,000 population; p trend< 0.01), despite all-cause hospitalizations beginning to decline after 2008 (Figure 1). Hospitalizations for CD were consistently more frequent than those with UC (Table 1). The proportion of hospitalizations significantly increased among individuals ≥60 years of age with CD and UC (p trend< 0.01), but remained stable in the non-IBD population; IBD-related hospitalizations for other age groups remained stable or declined. Over the two decades, there was a steady decline in proportion of hospitalizations of white CD and UC individuals and increase within each minority racial/ethnic demographic. There was no difference in hospitalizations based on gender.
Discussion: Over the past 20 years since the introduction of biologics for IBD, the numbers and proportions of hospitalizations for both UC and CD have increased, exceeding epidemiologic changes in all-cause hospitalizations and the US population. The proportion of hospitalizations increased for elderly (≥60) and non-white individuals, but remained stable for other demographics. These shifts in the IBD-related hospitalizations patterns likely reflect the increasing incidence and prevalence of IBD as well as the changing demographics of IBD.

Disclosures:
Ellen J. Spartz, MD, Vivy Cusumano, MD, Jenny Sauk, MD, Berkeley Limketkai, MD, PhD. P2227 - Longitudinal Trends in Inflammatory Bowel Disease Hospitalizations in the Era of Biologics: A 20 Year Nationwide Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
UCLA, Los Angeles, CA
Introduction: Infliximab was the first biologic approved for Crohn’s disease (CD) in 1998, heralding an era of powerful immunosuppressive therapies. Two decades later, there are 11 FDA-approved biologic agents and small molecule inhibitors for the management of inflammatory bowel disease (IBD). It remains unclear whether the availability of these agents has had an impact on hospitalizations, a surrogate for IBD disease severity and failure of outpatient medical treatments. The aim of this study was to examine the overall epidemiology and longitudinal trends of IBD-related hospitalizations in the era of biologics.
Methods: This retrospective study analyzed the National Inpatient Sample (NIS) databases from 1998-2018. Hospitalizations for ulcerative colitis (UC) and CD were identified by the International Classification of Diseases (ICD)-9 and 10 codes in the first 3 diagnosis positions. Hospitalization trends were evaluated according to time, age group (every 2 decades), sex, and race. Denominators included IBD-only hospitalizations, all-cause hospitalizations, and the United States (US) population.
Results: From 1998 through 2018, there was a rising trend for UC (14.0 to 26.0/100,000 population; p trend< 0.01) and CD hospitalizations (23.0 to 43.8/100,000 population; p trend< 0.01), despite all-cause hospitalizations beginning to decline after 2008 (Figure 1). Hospitalizations for CD were consistently more frequent than those with UC (Table 1). The proportion of hospitalizations significantly increased among individuals ≥60 years of age with CD and UC (p trend< 0.01), but remained stable in the non-IBD population; IBD-related hospitalizations for other age groups remained stable or declined. Over the two decades, there was a steady decline in proportion of hospitalizations of white CD and UC individuals and increase within each minority racial/ethnic demographic. There was no difference in hospitalizations based on gender.
Discussion: Over the past 20 years since the introduction of biologics for IBD, the numbers and proportions of hospitalizations for both UC and CD have increased, exceeding epidemiologic changes in all-cause hospitalizations and the US population. The proportion of hospitalizations increased for elderly (≥60) and non-white individuals, but remained stable for other demographics. These shifts in the IBD-related hospitalizations patterns likely reflect the increasing incidence and prevalence of IBD as well as the changing demographics of IBD.

Figure: Figure 1: Yearly trends of CD and UC hospitalizations
(A) Yearly trends of hospitalizations per 100,000 in US population and (B) per 10,000 all-cause hospitalizations. (C) CD hospitalization trends by age group. (D) UC hospitalizations by age group.
(A) Yearly trends of hospitalizations per 100,000 in US population and (B) per 10,000 all-cause hospitalizations. (C) CD hospitalization trends by age group. (D) UC hospitalizations by age group.
Disclosures:
Ellen Spartz indicated no relevant financial relationships.
Vivy Cusumano indicated no relevant financial relationships.
Jenny Sauk indicated no relevant financial relationships.
Berkeley Limketkai: Azora Therapeutics – Consultant, Stock-privately held company.
Ellen J. Spartz, MD, Vivy Cusumano, MD, Jenny Sauk, MD, Berkeley Limketkai, MD, PhD. P2227 - Longitudinal Trends in Inflammatory Bowel Disease Hospitalizations in the Era of Biologics: A 20 Year Nationwide Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
