Monday Poster Session
Category: IBD
P2239 - Gastrocolic Fistula: A Rare Anomalous Connection in Crohn’s Disease
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sherin Samuel, DO
University of Massachusetts Chan Medical School-Baystate
Springfield, MA
Presenting Author(s)
Sherin Samuel, DO1, Sharmeen Azher, MD1, Kevin Groudan, MD1, Ira Schmelkin, MD2
1University of Massachusetts Chan Medical School-Baystate, Springfield, MA; 2Baystate Health, Richmond, MA
Introduction: Gastrocolic fistulas are abnormal connections between the mucosal layers of the stomach and colon, most commonly the greater curvature and transverse colon. Majority of cases are secondary to abdominal surgery; the remaining 20% are in the setting of inflammatory conditions, rarely including Crohn’s disease. We present the unique case of a middle-aged man with longstanding Crohn’s disease on immunomodulatory treatment who presented with nonspecific symptoms and was found to have a gastrocolic fistula.
Case Description/Methods: A 49-year-old man with history of fistulizing Crohn’s disease status post Hartman procedure, managed on adalimumab and azathioprine presented with one month of worsening back pain radiating to his abdomen. The pain was not associated with fevers, chills, nausea or vomiting. He had normal output from his ostomy. He was vitally stable. His labs did not reveal leukocytosis. Imaging revealed a loculated fluid collection near the gastric antrum which was possibly connected with inflamed and thick-walled transverse colon with adjacent stranding. The patient was admitted to the colorectal surgery service and started on broad-spectrum antibiotics. Gastroenterology evaluation was requested. Endoscopy was performed to rule out gastric ulcer causing perforation as well as to assess for Crohn’s disease. It revealed a fistulous opening containing stool in the proximal gastric antrum. The patient underwent surgical intervention with exploratory laparotomy along with take down of colostomy, partial gastrectomy, repair of gastrocolic fistula, and creation of end ileostomy. After an uncomplicated post-op period, he was discharged with pain control and a one month course of metronidazole. He continued his immunomodulatory therapy on adalimumab with follow-up by his outpatient gastroenterology physician.
Discussion: Gastrocolic fistulas are a rare complication of Crohn’s disease. When symptomatic, 30% of patients can present with weight loss, vomiting of fecal contents, or defecation of undigested food. Workup involves both radiological and endoscopic tests; endoscopy is not diagnostic but allows assessment of disease complexity. Mainstay of treatment is surgical resection of the anomalous tract and portions of the affected organs, preventing further complications. Clinicians should be aware of this rare complication of Crohn’s disease as when not identified promptly, it can result in delays in diagnosis and management.

Disclosures:
Sherin Samuel, DO1, Sharmeen Azher, MD1, Kevin Groudan, MD1, Ira Schmelkin, MD2. P2239 - Gastrocolic Fistula: A Rare Anomalous Connection in Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Massachusetts Chan Medical School-Baystate, Springfield, MA; 2Baystate Health, Richmond, MA
Introduction: Gastrocolic fistulas are abnormal connections between the mucosal layers of the stomach and colon, most commonly the greater curvature and transverse colon. Majority of cases are secondary to abdominal surgery; the remaining 20% are in the setting of inflammatory conditions, rarely including Crohn’s disease. We present the unique case of a middle-aged man with longstanding Crohn’s disease on immunomodulatory treatment who presented with nonspecific symptoms and was found to have a gastrocolic fistula.
Case Description/Methods: A 49-year-old man with history of fistulizing Crohn’s disease status post Hartman procedure, managed on adalimumab and azathioprine presented with one month of worsening back pain radiating to his abdomen. The pain was not associated with fevers, chills, nausea or vomiting. He had normal output from his ostomy. He was vitally stable. His labs did not reveal leukocytosis. Imaging revealed a loculated fluid collection near the gastric antrum which was possibly connected with inflamed and thick-walled transverse colon with adjacent stranding. The patient was admitted to the colorectal surgery service and started on broad-spectrum antibiotics. Gastroenterology evaluation was requested. Endoscopy was performed to rule out gastric ulcer causing perforation as well as to assess for Crohn’s disease. It revealed a fistulous opening containing stool in the proximal gastric antrum. The patient underwent surgical intervention with exploratory laparotomy along with take down of colostomy, partial gastrectomy, repair of gastrocolic fistula, and creation of end ileostomy. After an uncomplicated post-op period, he was discharged with pain control and a one month course of metronidazole. He continued his immunomodulatory therapy on adalimumab with follow-up by his outpatient gastroenterology physician.
Discussion: Gastrocolic fistulas are a rare complication of Crohn’s disease. When symptomatic, 30% of patients can present with weight loss, vomiting of fecal contents, or defecation of undigested food. Workup involves both radiological and endoscopic tests; endoscopy is not diagnostic but allows assessment of disease complexity. Mainstay of treatment is surgical resection of the anomalous tract and portions of the affected organs, preventing further complications. Clinicians should be aware of this rare complication of Crohn’s disease as when not identified promptly, it can result in delays in diagnosis and management.

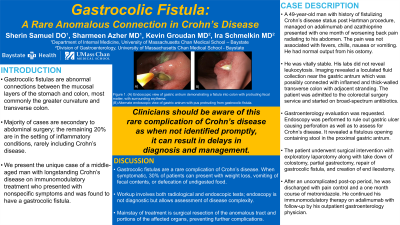
Figure: (A) Endoscopic view of gastric antrum demonstrating a fistula into colon with protruding fecal matter, with surrounding erythema.
(B) Alternate endoscopic view of gastric antrum with pus protruding from gastrocolic fistula.
(B) Alternate endoscopic view of gastric antrum with pus protruding from gastrocolic fistula.
Disclosures:
Sherin Samuel indicated no relevant financial relationships.
Sharmeen Azher indicated no relevant financial relationships.
Kevin Groudan indicated no relevant financial relationships.
Ira Schmelkin indicated no relevant financial relationships.
Sherin Samuel, DO1, Sharmeen Azher, MD1, Kevin Groudan, MD1, Ira Schmelkin, MD2. P2239 - Gastrocolic Fistula: A Rare Anomalous Connection in Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
