Monday Poster Session
Category: IBD
P2243 - Therapeutic Hemicolectomy for Intractable Hemorrhage in New-Onset Fistulizing Crohn’s Disease
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Alexander M. Carlson, DO
University at Buffalo
Buffalo, NY
Presenting Author(s)
Alexander M. Carlson, DO, Clive J. Miranda, DO, MS, Kevin Yang, MD, Gina Sparacino, MD, Mayada Ismail, MD
University at Buffalo, Buffalo, NY
Introduction: Certain patients with Crohn’s disease (CD) may experience a silent or asymptomatic disease progression over the course of several years. Here we present the case of a young, new-onset CD patient presenting with an atypical and severe clinical course, who underwent a therapeutic hemicolectomy for uncontrollable gastrointestinal bleeding.
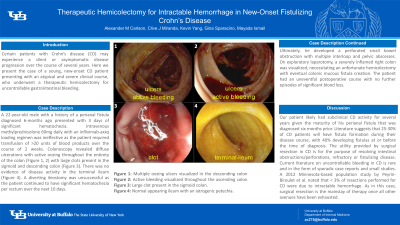
Case Description/Methods: A 22-year-old male with a history of a perianal fistula diagnosed 6-months ago presented with 3 days of significant hematochezia. Intravenous methylprednisolone 60mg daily with an infliximab-axxq loading regimen was ineffective as the patient required transfusion of >20 units of blood products over the course of 2 weeks. Colonoscopy revealed diffuse ulcerations with active oozing throughout the entirety of the colon (Figure 1, 2) with large clots present in the sigmoid and descending colon (Figure 3). There was no evidence of disease activity in the terminal ileum (Figure 4). A diverting ileostomy was unsuccessful as the patient continued to have significant hematochezia per rectum over the next 10 days. Ultimately, he developed a perforated small bowel obstruction with multiple interloop and pelvic abscesses. On exploratory laparotomy, a severely inflamed right colon was visualized, necessitating an unfortunate hemicolectomy with eventual colonic mucous fistula creation. The patient had an uneventful postoperative course with no further episodes of significant blood loss.
Discussion: Our patient likely had subclinical CD activity for several years given the maturity of his perianal fistula that was diagnosed six months prior. Literature suggests that 25-30% of CD patients will have fistula formation during their disease course, with 40% developing fistulas at or before the time of diagnosis. The utility provided by surgical resection in CD is for the purpose of resolving intestinal obstructions/perforations, refractory or fistulizing disease. Current literature on uncontrollable bleeding in CD is rare and in the form of sporadic case reports and small studies. A 2012 Minnesota-based population study by Peyrin-Biroulet et al. noted that < 3% of resections performed for CD were due to intractable hemorrhage. As in this case, surgical resection is the mainstay of therapy once all other avenues have been exhausted.
In summary, we describe a rare case of new-onset, fistulizing Crohn’s disease that presented as an uncontrollable hemorrhage, ultimately requiring a therapeutic hemicolectomy to prevent further blood loss.

Disclosures:
Alexander M. Carlson, DO, Clive J. Miranda, DO, MS, Kevin Yang, MD, Gina Sparacino, MD, Mayada Ismail, MD. P2243 - Therapeutic Hemicolectomy for Intractable Hemorrhage in New-Onset Fistulizing Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University at Buffalo, Buffalo, NY
Introduction: Certain patients with Crohn’s disease (CD) may experience a silent or asymptomatic disease progression over the course of several years. Here we present the case of a young, new-onset CD patient presenting with an atypical and severe clinical course, who underwent a therapeutic hemicolectomy for uncontrollable gastrointestinal bleeding.
Case Description/Methods: A 22-year-old male with a history of a perianal fistula diagnosed 6-months ago presented with 3 days of significant hematochezia. Intravenous methylprednisolone 60mg daily with an infliximab-axxq loading regimen was ineffective as the patient required transfusion of >20 units of blood products over the course of 2 weeks. Colonoscopy revealed diffuse ulcerations with active oozing throughout the entirety of the colon (Figure 1, 2) with large clots present in the sigmoid and descending colon (Figure 3). There was no evidence of disease activity in the terminal ileum (Figure 4). A diverting ileostomy was unsuccessful as the patient continued to have significant hematochezia per rectum over the next 10 days. Ultimately, he developed a perforated small bowel obstruction with multiple interloop and pelvic abscesses. On exploratory laparotomy, a severely inflamed right colon was visualized, necessitating an unfortunate hemicolectomy with eventual colonic mucous fistula creation. The patient had an uneventful postoperative course with no further episodes of significant blood loss.
Discussion: Our patient likely had subclinical CD activity for several years given the maturity of his perianal fistula that was diagnosed six months prior. Literature suggests that 25-30% of CD patients will have fistula formation during their disease course, with 40% developing fistulas at or before the time of diagnosis. The utility provided by surgical resection in CD is for the purpose of resolving intestinal obstructions/perforations, refractory or fistulizing disease. Current literature on uncontrollable bleeding in CD is rare and in the form of sporadic case reports and small studies. A 2012 Minnesota-based population study by Peyrin-Biroulet et al. noted that < 3% of resections performed for CD were due to intractable hemorrhage. As in this case, surgical resection is the mainstay of therapy once all other avenues have been exhausted.
In summary, we describe a rare case of new-onset, fistulizing Crohn’s disease that presented as an uncontrollable hemorrhage, ultimately requiring a therapeutic hemicolectomy to prevent further blood loss.

Figure: Figure 1: Multiple oozing ulcers visualized in the descending colon
Figure 2: Active bleeding visualized throughout the ascending colon
Figure 3: Large clot present in the sigmoid colon.
Figure 4: Normal appearing ileum with an iatrogenic petechia.
Figure 2: Active bleeding visualized throughout the ascending colon
Figure 3: Large clot present in the sigmoid colon.
Figure 4: Normal appearing ileum with an iatrogenic petechia.
Disclosures:
Alexander Carlson indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Kevin Yang indicated no relevant financial relationships.
Gina Sparacino indicated no relevant financial relationships.
Mayada Ismail indicated no relevant financial relationships.
Alexander M. Carlson, DO, Clive J. Miranda, DO, MS, Kevin Yang, MD, Gina Sparacino, MD, Mayada Ismail, MD. P2243 - Therapeutic Hemicolectomy for Intractable Hemorrhage in New-Onset Fistulizing Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
