Monday Poster Session
Category: IBD
P2245 - An Atypical Case of Yersinia enterocolitica Infection in a Patient Suspected With Ulcerative Colitis Flare-Up
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Priyam Doshi, MD, MPH
Western Reserve Hospital
Fairlawn, OH
Presenting Author(s)
Priyam Doshi, MD, MPH, Ghomathy Sivaram, MD, Corey Sievers, MD, Todd Lisy, MD
Western Reserve Hospital, Cuyahoga Falls, OH
Introduction: There is evidence that Ulcerative colitis (UC), a chronic immune-mediated inflammatory bowel disease (IBD), results from an inappropriate immune response to enteric microbes by causing a defective mucosal barrier in susceptible cases. Yersinia enterocolitica, is hypothesized to be one of the causes. The Center for Disease Control (CDC) estimates Yersinia causing almost 117,000 illnesses, 640 hospitalizations and 35 deaths in United States every year.
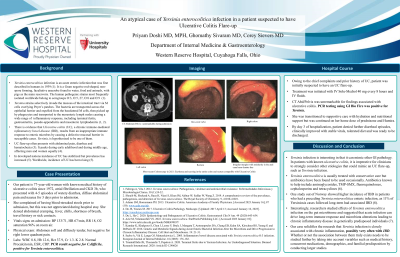
Case Description/Methods: The patient is 77-year-old woman with known medical history of ulcerative colitis since 1972, atrial fibrillation who presented with 4-5 episodes of watery diarrhea, diffuse abdominal pain and nausea for 3 days prior to admission. Vital signs on presentation were unremarkable. On physical exam, her abdomen was soft with diffused tenderness. White blood cell count was 8.8, hemoglobin 12.6, with creatinine of 1.3. She had normal procalcitonin, erythrocyte sedimentation rate and C-reactive protein. Owing to the chief complaints and prior history, she suspected to have an UC flare-up, and was started on IV Solu-Medrol 40 mg every 8 hours with IV fluids. CT abdomen/pelvis was unremarkable for findings of ulcerative colitis. Most recent colonoscopy report from 2021 showed mucosal nodularity, hyperemia and erosions. Her PCR testing using GI Bio Fire was positive for Yersinia. She was transitioned to supportive care with hydration and nutritional support but was continued on her chronic home dose of prednisone and Humira to prevent flare-ups. By day 3 of hospitalization, patient denied further diarrheal episodes, tolerated diet and was ready to be discharged.
Discussion: It has been suggested that acute infection can drive long-term immune response and microbiota alterations leading to chronic inflammatory disease in genetically predisposed individuals. Our case was unique because it could very likely be possible that our patient had Yersinia infection 50 years ago that went undiagnosed and may have triggered multiple immune responses leading to UC flare ups. At the same time, it could be possible that having ulcerative colitis was a risk factor for an enteric infection like Yersinia, especially when you consider that many patients with ulcerative colitis are on immunosuppressive drugs.

Disclosures:
Priyam Doshi, MD, MPH, Ghomathy Sivaram, MD, Corey Sievers, MD, Todd Lisy, MD. P2245 - An Atypical Case of Yersinia enterocolitica Infection in a Patient Suspected With Ulcerative Colitis Flare-Up, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Western Reserve Hospital, Cuyahoga Falls, OH
Introduction: There is evidence that Ulcerative colitis (UC), a chronic immune-mediated inflammatory bowel disease (IBD), results from an inappropriate immune response to enteric microbes by causing a defective mucosal barrier in susceptible cases. Yersinia enterocolitica, is hypothesized to be one of the causes. The Center for Disease Control (CDC) estimates Yersinia causing almost 117,000 illnesses, 640 hospitalizations and 35 deaths in United States every year.
Case Description/Methods: The patient is 77-year-old woman with known medical history of ulcerative colitis since 1972, atrial fibrillation who presented with 4-5 episodes of watery diarrhea, diffuse abdominal pain and nausea for 3 days prior to admission. Vital signs on presentation were unremarkable. On physical exam, her abdomen was soft with diffused tenderness. White blood cell count was 8.8, hemoglobin 12.6, with creatinine of 1.3. She had normal procalcitonin, erythrocyte sedimentation rate and C-reactive protein. Owing to the chief complaints and prior history, she suspected to have an UC flare-up, and was started on IV Solu-Medrol 40 mg every 8 hours with IV fluids. CT abdomen/pelvis was unremarkable for findings of ulcerative colitis. Most recent colonoscopy report from 2021 showed mucosal nodularity, hyperemia and erosions. Her PCR testing using GI Bio Fire was positive for Yersinia. She was transitioned to supportive care with hydration and nutritional support but was continued on her chronic home dose of prednisone and Humira to prevent flare-ups. By day 3 of hospitalization, patient denied further diarrheal episodes, tolerated diet and was ready to be discharged.
Discussion: It has been suggested that acute infection can drive long-term immune response and microbiota alterations leading to chronic inflammatory disease in genetically predisposed individuals. Our case was unique because it could very likely be possible that our patient had Yersinia infection 50 years ago that went undiagnosed and may have triggered multiple immune responses leading to UC flare ups. At the same time, it could be possible that having ulcerative colitis was a risk factor for an enteric infection like Yersinia, especially when you consider that many patients with ulcerative colitis are on immunosuppressive drugs.

Figure: CT Abdomen/Pelvis conducted during the time of admission
Disclosures:
Priyam Doshi indicated no relevant financial relationships.
Ghomathy Sivaram indicated no relevant financial relationships.
Corey Sievers indicated no relevant financial relationships.
Todd Lisy indicated no relevant financial relationships.
Priyam Doshi, MD, MPH, Ghomathy Sivaram, MD, Corey Sievers, MD, Todd Lisy, MD. P2245 - An Atypical Case of Yersinia enterocolitica Infection in a Patient Suspected With Ulcerative Colitis Flare-Up, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
