Monday Poster Session
Category: IBD
P2259 - Plasmablastic Lymphoma in a Patient with Treatment Refractory Ulcerative Colitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Abraham Ifrah, MD, MS
Temple University Hospital
Bala Cynwynd, PA
Presenting Author(s)
Abraham Ifrah, MD, MS1, Christopher Kasia, MD1, Yekaterina Belogrivtseva, MD1, Adam C. Ehrlich, MD, MPH2
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Plasmablastic lymphoma (PBL) is rare and aggressive with a survival rate less than 14 months. There have been 9 documented cases of PBL in Crohn's disease (CD) and 2 in ulcerative colitis (UC). Here we present the third case of PBL in UC and the first while on ustekinumab.
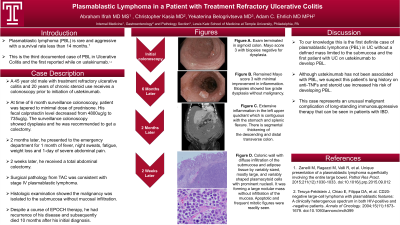
Case Description/Methods: A 45-year-old man with treatment-refractory ulcerative colitis on ustekinumab for 8 months presented to the emergency department for 1 month of fever, night sweats, fatigue, weight loss and 1-day of severe abdominal pain. His prior UC history included prior treatment failure to azathioprine, infliximab, adalimumab, golimumab, and tofacitinib. He had been treated with prednisone at varying doses for >20 years. He was started on ustekinumab with partial clinical response and successfully tapered off budesonide and to a minimal dose of prednisone. Fecal calprotectin improved from 4800ug/g to 735ug/g but follow-up colonoscopy remained Mayo score 3 with minimal improvement in inflammation (Fig A,B). Based on his refractory disease and presence of low grade dysplasia on biopsies, he underwent a total abdominal colectomy. Surgical pathology was consistent with stage IV PBL. Histologic examination showed the malignancy was isolated to the submucosa without mucosal infiltration (Fig F,G). Despite a course of EPOCH therapy, he had recurrence of his disease and subsequently died 10 months after his initial diagnosis.
Discussion: There are 2 previously reported cases of PBL in UC. To our knowledge this is the first definite case of PBL in UC without a defined mass limited to the submucosa and the first patient with UC on ustekinumab to develop PBL. While our patient had clinical improvement after starting ustekinumab, he had long-standing severe and refractory disease. Although ustekinumab has not been associated with PBL, we suspect this patient’s long history on anti-TNFs and steroid use increased his risk of developing PBL. This case represents an unusual malignant complication of long-standing immunosuppressive therapy that can be seen in patients with IBD.

Disclosures:
Abraham Ifrah, MD, MS1, Christopher Kasia, MD1, Yekaterina Belogrivtseva, MD1, Adam C. Ehrlich, MD, MPH2. P2259 - Plasmablastic Lymphoma in a Patient with Treatment Refractory Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Plasmablastic lymphoma (PBL) is rare and aggressive with a survival rate less than 14 months. There have been 9 documented cases of PBL in Crohn's disease (CD) and 2 in ulcerative colitis (UC). Here we present the third case of PBL in UC and the first while on ustekinumab.
Case Description/Methods: A 45-year-old man with treatment-refractory ulcerative colitis on ustekinumab for 8 months presented to the emergency department for 1 month of fever, night sweats, fatigue, weight loss and 1-day of severe abdominal pain. His prior UC history included prior treatment failure to azathioprine, infliximab, adalimumab, golimumab, and tofacitinib. He had been treated with prednisone at varying doses for >20 years. He was started on ustekinumab with partial clinical response and successfully tapered off budesonide and to a minimal dose of prednisone. Fecal calprotectin improved from 4800ug/g to 735ug/g but follow-up colonoscopy remained Mayo score 3 with minimal improvement in inflammation (Fig A,B). Based on his refractory disease and presence of low grade dysplasia on biopsies, he underwent a total abdominal colectomy. Surgical pathology was consistent with stage IV PBL. Histologic examination showed the malignancy was isolated to the submucosa without mucosal infiltration (Fig F,G). Despite a course of EPOCH therapy, he had recurrence of his disease and subsequently died 10 months after his initial diagnosis.
Discussion: There are 2 previously reported cases of PBL in UC. To our knowledge this is the first definite case of PBL in UC without a defined mass limited to the submucosa and the first patient with UC on ustekinumab to develop PBL. While our patient had clinical improvement after starting ustekinumab, he had long-standing severe and refractory disease. Although ustekinumab has not been associated with PBL, we suspect this patient’s long history on anti-TNFs and steroid use increased his risk of developing PBL. This case represents an unusual malignant complication of long-standing immunosuppressive therapy that can be seen in patients with IBD.

Figure: A and B. Representative Colonoscopy Images. C, D and E. Representative Coronal CT Images. F. Plasmablastic Lymphoma at Low Magnification. G. Plasmablastic Lymphoma at High Magnification.
Disclosures:
Abraham Ifrah indicated no relevant financial relationships.
Christopher Kasia indicated no relevant financial relationships.
Yekaterina Belogrivtseva indicated no relevant financial relationships.
Adam Ehrlich: Abbvie – Advisor or Review Panel Member. Bristol Meyers Squibb – Advisor or Review Panel Member. Eli Lilly – Advisor or Review Panel Member.
Abraham Ifrah, MD, MS1, Christopher Kasia, MD1, Yekaterina Belogrivtseva, MD1, Adam C. Ehrlich, MD, MPH2. P2259 - Plasmablastic Lymphoma in a Patient with Treatment Refractory Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
