Monday Poster Session
Category: IBD
P2264 - Intestinal Ganglioneuromatosis: A Rare Mimic of Inflammatory Bowel Disease
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- AN
Andrea Noronha, BS
Lewis Katz School of Medicine
Philadelphia, PA
Presenting Author(s)
Andrea Noronha, BS1, Imran Siddiqui, MD2
1Lewis Katz School of Medicine, Philadelphia, PA; 2Desert Valley Hospital, Victorville, CA
Introduction: Intestinal ganglioneuromatosis (IG) is a rare disorder characterized by hamartomatous proliferation of glial and neuronal elements of the enteric plexuses. It can occur in any part of the gastrointestinal tract, but most commonly affects the ileum, colon and appendix.
Case Description/Methods: A 51-year-old female presented with history of 12-pound weight loss, bloating and abdominal distension. She denied diarrhea, constipation or abdominal pain. She also had history of hypertension, uncontrolled diabetes and obesity. Colonoscopy revealed “mild to moderate diffuse ulcerative colitis with superficial aphthous-like ulcerations and pseudopolyps more prominent in the left colon” and sigmoid stricture with mucosal edema and erythema. There was relative sparing of the rectum. Patient was immediately started on a trial of mesalamine and steroids. However, biopsies of the right, left and sigmoid colon all revealed fragments of colonic mucosa with foci of spindle cell proliferation within a fibrillary matrix with intermixed ganglion cells, expanding the lamina propria. Focally the proliferation pushed and distorted the crypts. No basal plasmacytosis, active inflammation or granulomas were seen. Immunohistochemical stains revealed these cells to be positive with S100, SOX10 and synaptophysin and negative with CD34, CD117, DOG1 as well as negative with epithelial and smooth muscle markers. The findings were consistent with intestinal ganglioneuromatosis.
Discussion: IG is divided into 3 types: polypoid ganglioneuroma, ganglioneuromatous polyposis and diffuse ganglioneuromatosis. Ganglioneuromatous proliferations arising from the myenteric plexus in the muscularis propria can lead to mural thickening and strictures. The proliferation may also arise from the submucosal Meissner’s plexus, extending into and expanding the lamina propria resulting in mucosal friability and erosion. Polypoid proliferation can mimic pseudopolyps. All these can result in a mistaken impression of inflammatory bowel disease (IBD) as in our case. Unlike IBD, treatment for IG is surgical excision of affected segments, if symptoms are severe. Additionally, diffuse ganglioneuromatosis has syndromic associations with Neurofibromatosis type 1 and Multiple Endocrine Neoplasia (MEN) IIB. Polypoid ganglioneuromatosis is associated with phosphatase and tensin homolog (PTEN) hamartoma tumor syndrome (which includes Cowden syndrome). Therefore, proper work-up to exclude syndromic associations is important.

Disclosures:
Andrea Noronha, BS1, Imran Siddiqui, MD2. P2264 - Intestinal Ganglioneuromatosis: A Rare Mimic of Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Lewis Katz School of Medicine, Philadelphia, PA; 2Desert Valley Hospital, Victorville, CA
Introduction: Intestinal ganglioneuromatosis (IG) is a rare disorder characterized by hamartomatous proliferation of glial and neuronal elements of the enteric plexuses. It can occur in any part of the gastrointestinal tract, but most commonly affects the ileum, colon and appendix.
Case Description/Methods: A 51-year-old female presented with history of 12-pound weight loss, bloating and abdominal distension. She denied diarrhea, constipation or abdominal pain. She also had history of hypertension, uncontrolled diabetes and obesity. Colonoscopy revealed “mild to moderate diffuse ulcerative colitis with superficial aphthous-like ulcerations and pseudopolyps more prominent in the left colon” and sigmoid stricture with mucosal edema and erythema. There was relative sparing of the rectum. Patient was immediately started on a trial of mesalamine and steroids. However, biopsies of the right, left and sigmoid colon all revealed fragments of colonic mucosa with foci of spindle cell proliferation within a fibrillary matrix with intermixed ganglion cells, expanding the lamina propria. Focally the proliferation pushed and distorted the crypts. No basal plasmacytosis, active inflammation or granulomas were seen. Immunohistochemical stains revealed these cells to be positive with S100, SOX10 and synaptophysin and negative with CD34, CD117, DOG1 as well as negative with epithelial and smooth muscle markers. The findings were consistent with intestinal ganglioneuromatosis.
Discussion: IG is divided into 3 types: polypoid ganglioneuroma, ganglioneuromatous polyposis and diffuse ganglioneuromatosis. Ganglioneuromatous proliferations arising from the myenteric plexus in the muscularis propria can lead to mural thickening and strictures. The proliferation may also arise from the submucosal Meissner’s plexus, extending into and expanding the lamina propria resulting in mucosal friability and erosion. Polypoid proliferation can mimic pseudopolyps. All these can result in a mistaken impression of inflammatory bowel disease (IBD) as in our case. Unlike IBD, treatment for IG is surgical excision of affected segments, if symptoms are severe. Additionally, diffuse ganglioneuromatosis has syndromic associations with Neurofibromatosis type 1 and Multiple Endocrine Neoplasia (MEN) IIB. Polypoid ganglioneuromatosis is associated with phosphatase and tensin homolog (PTEN) hamartoma tumor syndrome (which includes Cowden syndrome). Therefore, proper work-up to exclude syndromic associations is important.

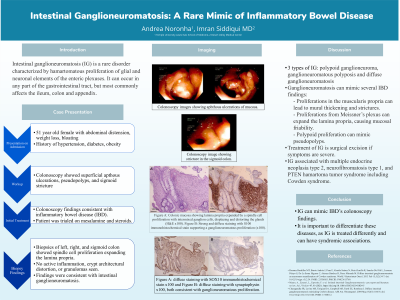
Figure: Figure A: Colonic mucosa showing lamina propria expanded by a spindle cell proliferation with intermixed ganglion cells, displacing and distorting the glands (H&E x100).
Figure B: Strong and diffuse staining with S100 immunohistochemical stain supporting a ganglioneuromatous proliferation (x100).
Figure C: Colonoscopy image showing stricture with erythema and ulceration of overlying mucosa.
Figure B: Strong and diffuse staining with S100 immunohistochemical stain supporting a ganglioneuromatous proliferation (x100).
Figure C: Colonoscopy image showing stricture with erythema and ulceration of overlying mucosa.
Disclosures:
Andrea Noronha indicated no relevant financial relationships.
Imran Siddiqui indicated no relevant financial relationships.
Andrea Noronha, BS1, Imran Siddiqui, MD2. P2264 - Intestinal Ganglioneuromatosis: A Rare Mimic of Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
