Monday Poster Session
Category: Interventional Endoscopy
P2276 - Endoscopic vs Surgical Ampullectomy for Ampullary Adenomas: A Systematic Review and Meta-Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Kwabena O. Asafo-Agyei, MD
Christus Highland Hospital
Shreveport, LA
Presenting Author(s)
Samuel Igbinedion, MD1, Nkengeh Tazinkeng, MD2, Kwabena O. Asafo-Agyei, MD3, Chukwunonso B. Ezeani, MBBS4, Ikechukwu Eze, MD5, Carol Mita, 6, Douglas Pleskow, MD, FACG7, Mandeep Sawhney, MD, MS8, Tyler Berzin, MD, FACG8, Moamen Gabr, MD, MSc,8
1Beth Israel Deaconess Medical Center, Harvard Medical School, Quincy, MA; 2African Association of Future Gastroenterologists, Buea, Sud-Ouest, Cameroon; 3Christus Highland Hospital, Shreveport, LA; 4Baton Rouge General Hospital, Baton Rouge, LA; 5Howard University Hospital, Washington, DC; 6Harvard Medical School, Boston, MA; 7BIDMC, Boston, MA; 8Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Ampullary adenomas are benign neoplasms that have malignant potential. The risk of ampullary adenomas and carcinomas is increased almost 300 fold in patients with genetic polyposis syndromes. Complete resection is necessary to prevent malignant transformation. Endoscopy and surgery approaches are two disctinct methods of resection. Local resection with endoscopic ampullectomy has a recurrence rate of up to 30% and requires the burden of surveillance. Surgical methods which include transduodenal ampullectomy and pancreaticoduodenectomy are invasive with higher morbidity (25 – 65%) and mortality (0 – 10%) rates. Recent literature has demonstrated safety and efficacy of endoscopic ampullectomy in comparison with surgery. We performed a meta-analysis of the studies comparing endoscopic and surgical ampullectomy treatment approaches for ampullary adenomas.
Methods: A comprehensive search of multiple databases like Cochrane library, PubMed, EMBASE, and Web of Science (from inception to March 2023) was conducted for studies comparing surgery and endoscopic ampullectomy for ampullary adenoma. The primary outcome in our study was complication rate with a focus on infection. Other outcomes were recurrence and complete resection rates. We used meta-analysis techniques to calculate pooled estimates using the random effects model. Heterogeneity was assessed using I2 statistic. We also calculated a 95% prediction interval. All analyses were performed by using Comprehensive Meta-Analysis software, version 4 (BioStat, Englewood, NJ)
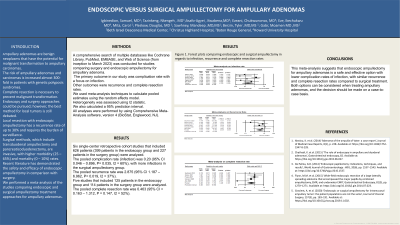
Results: Six single-center retrospective cohort studies that included 626 patients (399 patients in endoscopy group and 227 patients in surgery group) were analyzed. The pooled complication rate (infection) was 0.20 (95% CI 0.046 – 0.896, P= 0.035, I2 = 60%), with more infections in the surgical ampullectomy group. The pooled recurrence rate was 2.875 (95% CI 1.187 – 6.962, P= 0.019, I2 = 37%). Five studies that included 125 patients in the endoscopy group and 114 patients in the surgery group were analyzed. The pooled complete resection rate was 0.463 (95% CI = 0.163 – 1.312, P = 0.147, I2 = 52%)
Discussion: This meta-analysis suggests that endoscopic ampullectomy for ampullary adenomas is a safe and effective option with lower complication rates of infection, with similar recurrence and complete resection rates compared to surgical treatment. Both options can be considered when treating ampullary adenomas and the decision should be made by case to case basis

Disclosures:
Samuel Igbinedion, MD1, Nkengeh Tazinkeng, MD2, Kwabena O. Asafo-Agyei, MD3, Chukwunonso B. Ezeani, MBBS4, Ikechukwu Eze, MD5, Carol Mita, 6, Douglas Pleskow, MD, FACG7, Mandeep Sawhney, MD, MS8, Tyler Berzin, MD, FACG8, Moamen Gabr, MD, MSc,8. P2276 - Endoscopic vs Surgical Ampullectomy for Ampullary Adenomas: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Harvard Medical School, Quincy, MA; 2African Association of Future Gastroenterologists, Buea, Sud-Ouest, Cameroon; 3Christus Highland Hospital, Shreveport, LA; 4Baton Rouge General Hospital, Baton Rouge, LA; 5Howard University Hospital, Washington, DC; 6Harvard Medical School, Boston, MA; 7BIDMC, Boston, MA; 8Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Ampullary adenomas are benign neoplasms that have malignant potential. The risk of ampullary adenomas and carcinomas is increased almost 300 fold in patients with genetic polyposis syndromes. Complete resection is necessary to prevent malignant transformation. Endoscopy and surgery approaches are two disctinct methods of resection. Local resection with endoscopic ampullectomy has a recurrence rate of up to 30% and requires the burden of surveillance. Surgical methods which include transduodenal ampullectomy and pancreaticoduodenectomy are invasive with higher morbidity (25 – 65%) and mortality (0 – 10%) rates. Recent literature has demonstrated safety and efficacy of endoscopic ampullectomy in comparison with surgery. We performed a meta-analysis of the studies comparing endoscopic and surgical ampullectomy treatment approaches for ampullary adenomas.
Methods: A comprehensive search of multiple databases like Cochrane library, PubMed, EMBASE, and Web of Science (from inception to March 2023) was conducted for studies comparing surgery and endoscopic ampullectomy for ampullary adenoma. The primary outcome in our study was complication rate with a focus on infection. Other outcomes were recurrence and complete resection rates. We used meta-analysis techniques to calculate pooled estimates using the random effects model. Heterogeneity was assessed using I2 statistic. We also calculated a 95% prediction interval. All analyses were performed by using Comprehensive Meta-Analysis software, version 4 (BioStat, Englewood, NJ)
Results: Six single-center retrospective cohort studies that included 626 patients (399 patients in endoscopy group and 227 patients in surgery group) were analyzed. The pooled complication rate (infection) was 0.20 (95% CI 0.046 – 0.896, P= 0.035, I2 = 60%), with more infections in the surgical ampullectomy group. The pooled recurrence rate was 2.875 (95% CI 1.187 – 6.962, P= 0.019, I2 = 37%). Five studies that included 125 patients in the endoscopy group and 114 patients in the surgery group were analyzed. The pooled complete resection rate was 0.463 (95% CI = 0.163 – 1.312, P = 0.147, I2 = 52%)
Discussion: This meta-analysis suggests that endoscopic ampullectomy for ampullary adenomas is a safe and effective option with lower complication rates of infection, with similar recurrence and complete resection rates compared to surgical treatment. Both options can be considered when treating ampullary adenomas and the decision should be made by case to case basis

Figure: Forest plots comparing endoscopic and surgical ampullectomy in regards to infection, recurrence and complete resection rates
Disclosures:
Samuel Igbinedion indicated no relevant financial relationships.
Nkengeh Tazinkeng indicated no relevant financial relationships.
Kwabena Asafo-Agyei indicated no relevant financial relationships.
Chukwunonso Ezeani indicated no relevant financial relationships.
Ikechukwu Eze indicated no relevant financial relationships.
Carol Mita indicated no relevant financial relationships.
Douglas Pleskow: Boston Scientific – Consultant. Fuji – Consultant. Olympus – Consultant.
Mandeep Sawhney: Allurion – Stock Options. Immunovia Inc. – Consultant. Marlborough, MA – Consultant.
Tyler Berzin: Boston Scientific – Consultant. Fuji – Consultant. Medtronic – Consultant.
Moamen Gabr: Adaptive Endo – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Fuji – Consultant. Medtronic – Consultant. Olympus – Consultant.
Samuel Igbinedion, MD1, Nkengeh Tazinkeng, MD2, Kwabena O. Asafo-Agyei, MD3, Chukwunonso B. Ezeani, MBBS4, Ikechukwu Eze, MD5, Carol Mita, 6, Douglas Pleskow, MD, FACG7, Mandeep Sawhney, MD, MS8, Tyler Berzin, MD, FACG8, Moamen Gabr, MD, MSc,8. P2276 - Endoscopic vs Surgical Ampullectomy for Ampullary Adenomas: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

