Monday Poster Session
Category: Interventional Endoscopy
P2286 - Post Endoscopic Mucosal Resection Bleeding Risk with Antiplatelet or Anticoagulant Use: A Propensity-Matched Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- CN
Chengu Niu, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Chengu Niu, MD1, Kaiwen Zhu, MD1, Jing Zhang, MD2, Muhammad Farhan Ashraf, MD1, Tausif Syed, MD1, Karin Dunnigan, MD1
1Rochester General Hospital, Rochester, NY; 2Rainier Springs Hospital, Vancouver, WA
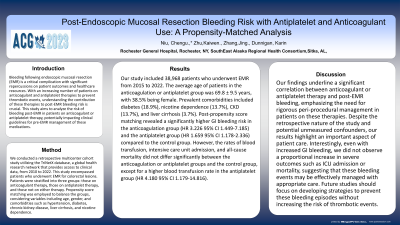
Introduction: Bleeding following endoscopic mucosal resection (EMR) is a critical complication with significant repercussions on patient outcomes and healthcare resources. With an increasing number of patients on anticoagulant and antiplatelet therapies to prevent thrombotic events, understanding the contribution of these therapies to post-EMR bleeding risk is crucial. This study aims to analyze the risk of bleeding post-EMR in patients on anticoagulant or antiplatelet therapy, potentially impacting clinical guidelines for pre-EMR management of these medications.
Methods: We conducted a retrospective multicenter cohort study utilizing the TriNetX database, a global health research network that provides access to clinical data, from 2010 to 2022. This study encompassed patients who underwent EMR for colorectal lesions. Patients were stratified into three groups: those on anticoagulant therapy, those on antiplatelet therapy, and those not on either therapy. Propensity score matching was employed to balance the groups.
Results: Our study included 38,968 patients who underwent EMR from 2010 to 2022. The average age of patients in the anticoagulation or antiplatelet group was 69.8 ± 9.5 years, with 38.5% being female. Prevalent comorbidities included diabetes (18.9%), nicotine dependence (13.7%), CKD (13.7%), and liver cirrhosis (3.7%). Post-propensity score matching revealed a significantly higher GI bleeding risk in the anticoagulation group (HR 3.226 95% CI 1.449-7.185) and the antiplatelet group (HR 1.659 95% CI 1.178-2.336) compared to the control group. However, the rates of blood transfusion, intensive care unit admission, and all-cause mortality did not differ significantly between the anticoagulation or antiplatelet groups and the control group, except for a higher blood transfusion rate in the antiplatelet group (HR 4.180 95% CI 1.179-14.816).
Discussion: Our findings underline a significant correlation between anticoagulant or antiplatelet therapy and post-EMR bleeding, emphasizing the need for rigorous peri-procedural management in patients on these therapies. Despite the retrospective nature of the study and potential unmeasured confounders, our results highlight an important aspect of patient care. Interestingly, even with increased GI bleeding, we did not observe a proportional increase in severe outcomes such as ICU admission or mortality, suggesting that these bleeding events may be effectively managed with appropriate care.
Disclosures:
Chengu Niu, MD1, Kaiwen Zhu, MD1, Jing Zhang, MD2, Muhammad Farhan Ashraf, MD1, Tausif Syed, MD1, Karin Dunnigan, MD1. P2286 - Post Endoscopic Mucosal Resection Bleeding Risk with Antiplatelet or Anticoagulant Use: A Propensity-Matched Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Rainier Springs Hospital, Vancouver, WA
Introduction: Bleeding following endoscopic mucosal resection (EMR) is a critical complication with significant repercussions on patient outcomes and healthcare resources. With an increasing number of patients on anticoagulant and antiplatelet therapies to prevent thrombotic events, understanding the contribution of these therapies to post-EMR bleeding risk is crucial. This study aims to analyze the risk of bleeding post-EMR in patients on anticoagulant or antiplatelet therapy, potentially impacting clinical guidelines for pre-EMR management of these medications.
Methods: We conducted a retrospective multicenter cohort study utilizing the TriNetX database, a global health research network that provides access to clinical data, from 2010 to 2022. This study encompassed patients who underwent EMR for colorectal lesions. Patients were stratified into three groups: those on anticoagulant therapy, those on antiplatelet therapy, and those not on either therapy. Propensity score matching was employed to balance the groups.
Results: Our study included 38,968 patients who underwent EMR from 2010 to 2022. The average age of patients in the anticoagulation or antiplatelet group was 69.8 ± 9.5 years, with 38.5% being female. Prevalent comorbidities included diabetes (18.9%), nicotine dependence (13.7%), CKD (13.7%), and liver cirrhosis (3.7%). Post-propensity score matching revealed a significantly higher GI bleeding risk in the anticoagulation group (HR 3.226 95% CI 1.449-7.185) and the antiplatelet group (HR 1.659 95% CI 1.178-2.336) compared to the control group. However, the rates of blood transfusion, intensive care unit admission, and all-cause mortality did not differ significantly between the anticoagulation or antiplatelet groups and the control group, except for a higher blood transfusion rate in the antiplatelet group (HR 4.180 95% CI 1.179-14.816).
Discussion: Our findings underline a significant correlation between anticoagulant or antiplatelet therapy and post-EMR bleeding, emphasizing the need for rigorous peri-procedural management in patients on these therapies. Despite the retrospective nature of the study and potential unmeasured confounders, our results highlight an important aspect of patient care. Interestingly, even with increased GI bleeding, we did not observe a proportional increase in severe outcomes such as ICU admission or mortality, suggesting that these bleeding events may be effectively managed with appropriate care.
Disclosures:
Chengu Niu indicated no relevant financial relationships.
Kaiwen Zhu indicated no relevant financial relationships.
Jing Zhang indicated no relevant financial relationships.
Muhammad Farhan Ashraf indicated no relevant financial relationships.
Tausif Syed indicated no relevant financial relationships.
Karin Dunnigan indicated no relevant financial relationships.
Chengu Niu, MD1, Kaiwen Zhu, MD1, Jing Zhang, MD2, Muhammad Farhan Ashraf, MD1, Tausif Syed, MD1, Karin Dunnigan, MD1. P2286 - Post Endoscopic Mucosal Resection Bleeding Risk with Antiplatelet or Anticoagulant Use: A Propensity-Matched Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
