Monday Poster Session
Category: Interventional Endoscopy
P2321 - Lynch- Not a Cinch: Hereditary Metastatic Breast Cancer With Diffuse GI Involvement
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sophia Christiansen
Brooke Army Medical Center
San Antonio, TX
Presenting Author(s)
Award: Presidential Poster Award
Sophia Christiansen, 1, Carl Kay, MD2, Cyrus Edelson, MD3, Shane Sweeny, MD1, John Magulick, MD1, Charles Miller, MD2
1Brooke Army Medical Center, San Antonio, TX; 2San Antonio Uniformed Services Health Education Consortium (SAUSHEC), San Antonio, TX; 3Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Metastatic breast cancer involving ascites is well-described, but luminal gastrointestinal (GI) tract involvement is less common and difficult to recognize given nonspecific symptoms. Invasive lobular breast cancer, which represents only 8% of breast cancers, is the type most likely to metastasize to the colon, duodenum, and stomach. However, there is a paucity of literature describing diagnosis of diffuse GI metastasis of breast cancer that is radiographically absent from the breasts.
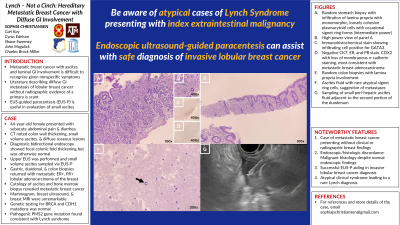
Case Description/Methods: A 44-year-old female presented with subacute abdominal pain and diarrhea. She was found to have CT evidence of colon wall thickening, small volume ascites, and diffuse osseous lesions. She underwent diagnostic bidirectional endoscopy as well as upper endoscopic ultrasound (EUS) to assess for free fluid. EUS showed a normal pancreas and biliary tree, as well as peri-hepatic ascites. Given concern for malignancy, ascites was sampled via EUS FNA (EUS-paracentesis; EUS-P). Endoscopic evaluation was mostly unremarkable save for thickened folds in the ascending colon. Given abdominal discomfort and diarrhea, random gastric, duodenal, and colon biopsies were obtained and returned with metastatic estrogen receptor +, progesterone receptor + lobular adenocarcinoma of the breast (Fig 1A-1E). Cytology on the ascites revealed metastatic breast cancer (Fig 1F). Bone marrow biopsy also returned with metastatic breast cancer. She had a mammogram, breast ultrasound, and breast MRI which were all unremarkable. Genetic testing revealed normal BRCA and CDH1 testing, but pathogenic mutation in PMS2 gene consistent with Lynch syndrome. After expert consultation, she was started on palliative chemotherapy for metastatic ER-positive breast cancer.
Discussion: This case combines four noteworthy features including: 1) metastatic disease without breast findings, 2) malignant histology despite normal endoscopy, 3) successful EUS-P aiding in invasive lobular breast cancer diagnosis, and 4) atypical clinical syndrome leading to a rare Lynch diagnosis. A niche for EUS-P has been described for small volume malignant ascites diagnoses, but this is one of the first cases of EUS-P utilized for safe diagnosis of invasive lobular breast cancer. As such, EUS-P should be part of the armamentarium of any gastroenterologist trained in EUS. Furthermore, hereditary cancer syndromes are rare, and presentations are variable. We highlight breast cancer as an index extraintestinal malignancy prompting diagnosis of Lynch syndrome.

Disclosures:
Sophia Christiansen, 1, Carl Kay, MD2, Cyrus Edelson, MD3, Shane Sweeny, MD1, John Magulick, MD1, Charles Miller, MD2. P2321 - Lynch- Not a Cinch: Hereditary Metastatic Breast Cancer With Diffuse GI Involvement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Sophia Christiansen, 1, Carl Kay, MD2, Cyrus Edelson, MD3, Shane Sweeny, MD1, John Magulick, MD1, Charles Miller, MD2
1Brooke Army Medical Center, San Antonio, TX; 2San Antonio Uniformed Services Health Education Consortium (SAUSHEC), San Antonio, TX; 3Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Metastatic breast cancer involving ascites is well-described, but luminal gastrointestinal (GI) tract involvement is less common and difficult to recognize given nonspecific symptoms. Invasive lobular breast cancer, which represents only 8% of breast cancers, is the type most likely to metastasize to the colon, duodenum, and stomach. However, there is a paucity of literature describing diagnosis of diffuse GI metastasis of breast cancer that is radiographically absent from the breasts.
Case Description/Methods: A 44-year-old female presented with subacute abdominal pain and diarrhea. She was found to have CT evidence of colon wall thickening, small volume ascites, and diffuse osseous lesions. She underwent diagnostic bidirectional endoscopy as well as upper endoscopic ultrasound (EUS) to assess for free fluid. EUS showed a normal pancreas and biliary tree, as well as peri-hepatic ascites. Given concern for malignancy, ascites was sampled via EUS FNA (EUS-paracentesis; EUS-P). Endoscopic evaluation was mostly unremarkable save for thickened folds in the ascending colon. Given abdominal discomfort and diarrhea, random gastric, duodenal, and colon biopsies were obtained and returned with metastatic estrogen receptor +, progesterone receptor + lobular adenocarcinoma of the breast (Fig 1A-1E). Cytology on the ascites revealed metastatic breast cancer (Fig 1F). Bone marrow biopsy also returned with metastatic breast cancer. She had a mammogram, breast ultrasound, and breast MRI which were all unremarkable. Genetic testing revealed normal BRCA and CDH1 testing, but pathogenic mutation in PMS2 gene consistent with Lynch syndrome. After expert consultation, she was started on palliative chemotherapy for metastatic ER-positive breast cancer.
Discussion: This case combines four noteworthy features including: 1) metastatic disease without breast findings, 2) malignant histology despite normal endoscopy, 3) successful EUS-P aiding in invasive lobular breast cancer diagnosis, and 4) atypical clinical syndrome leading to a rare Lynch diagnosis. A niche for EUS-P has been described for small volume malignant ascites diagnoses, but this is one of the first cases of EUS-P utilized for safe diagnosis of invasive lobular breast cancer. As such, EUS-P should be part of the armamentarium of any gastroenterologist trained in EUS. Furthermore, hereditary cancer syndromes are rare, and presentations are variable. We highlight breast cancer as an index extraintestinal malignancy prompting diagnosis of Lynch syndrome.

Figure: Figure 1: Microscopic images from random stomach biopsy at intermediate (1A, 100x magnification, H&E) and high (1B, 400x magnification, H&E) power magnifications showing infiltration of the lamina propria with monomorphic, loosely cohesive plasmacytoid cells with occasional signet ring forms present. Immunohistochemical staining revealed that the infiltrating cells were positive for GATA3 (1C, 400x magnification), CK7, ER, and PR and were negative for CDX2 (1D, 400x magnification) with loss of membranous e-cadherin staining, most consistent with a metastatic breast primary. Random colon biopsies (1E, 100x magnification, H&E) showed involvement of the lamina propria with similar cells, without significant surface epithelial abnormalities. Furthermore, microscopic examination of ascites fluid showed extremely rare atypical signet ring cells (200x magnification, H&E cell block), suggestive of metastatic involvement. Linear endoscopic ultrasound-guided 22-gauge needle sampling image (1G) showing sampling of small peri-hepatic ascites fluid adjacent to the second portion of the duodenum.
Disclosures:
Sophia Christiansen indicated no relevant financial relationships.
Carl Kay indicated no relevant financial relationships.
Cyrus Edelson indicated no relevant financial relationships.
Shane Sweeny indicated no relevant financial relationships.
John Magulick indicated no relevant financial relationships.
Charles Miller indicated no relevant financial relationships.
Sophia Christiansen, 1, Carl Kay, MD2, Cyrus Edelson, MD3, Shane Sweeny, MD1, John Magulick, MD1, Charles Miller, MD2. P2321 - Lynch- Not a Cinch: Hereditary Metastatic Breast Cancer With Diffuse GI Involvement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

