Monday Poster Session
Category: Interventional Endoscopy
P2326 - Clipping the Culprit: Management of a Gastrogastric Fistula Using Mucosectomy and an Over-the-Scope Clip
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Brent J. Gawey, MD, MSc
Mayo Clinic
Rochester, MN
Presenting Author(s)
Brent J. Gawey, MD, MSc, Khushboo Gala, MBBS, Mark Hanscom, MD, Barham Abu Dayyeh, MD, MPH
Mayo Clinic, Rochester, MN
Introduction: A gastrogastric fistula (GGF) is an abnormal connection between the stomach and a surgically created stomach pouch, often occurring as a complication of gastric bypass surgery. Timely and effective management has important prognostic implications. This case highlights a minimally invasive endoscopic approach for GGF closure. The aim is to further discuss this technique as an alternative to surgical management of GGFs.
Case Description/Methods: A 53-year-old female with comorbid obesity and steatohepatitis presented for evaluation of worsening reflux following Roux-en-Y gastric bypass (RYGB) 14 years prior. Her RYGB was complicated by a leak at the gastrojejunal anastomosis, necessitating reoperation. The patient's reflux was unresponsive to esomeprazole 40 mg twice daily. Esophagogastroduodenoscopy (EGD) and esophagram identified a GGF, thought to be contributing to the patient’s symptoms.
Both gastroenterology and bariatric surgery teams assessed the patient, discussing endoscopic and surgical closure options. The patient favored an endoscopic approach due to the high risk of requiring conversion to esophagojejunostomy if the fistula was surgically addressed, given its location near the gastroesophageal junction.
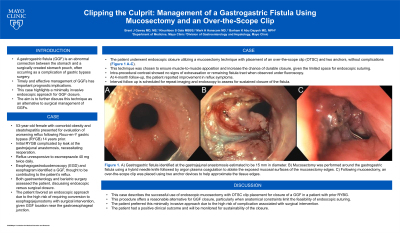
The patient underwent endoscopic closure utilizing a mucosectomy technique with placement of an over-the-scope clip (OTSC) and two anchors, without complications (Figure 1 A-C). This technique was chosen to ensure muscle-to-muscle apposition and increase the chance of durable closure, given the limited space for endoscopic suturing. Intra-procedural contrast showed no signs of extravasation or remaining fistula tract when observed under fluoroscopy. At 4-month follow-up, the patient reported improvement in reflux symptoms. She is scheduled for repeat imaging and endoscopy to assess for sustained closure of the fistula.
Discussion: This case describes the successful use of endoscopic mucosectomy with OTSC clip placement for closure of a GGF in a patient with prior RYBG. This procedure offers a reasonable alternative for GGF closure, particularly when anatomical constraints limit the feasibility of endoscopic suturing. The patient preferred this minimally invasive approach due to the high risk of complications associated with surgical intervention. The patient had a positive clinical outcome and will be closely monitored for sustainability of the closure.

Disclosures:
Brent J. Gawey, MD, MSc, Khushboo Gala, MBBS, Mark Hanscom, MD, Barham Abu Dayyeh, MD, MPH. P2326 - Clipping the Culprit: Management of a Gastrogastric Fistula Using Mucosectomy and an Over-the-Scope Clip, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: A gastrogastric fistula (GGF) is an abnormal connection between the stomach and a surgically created stomach pouch, often occurring as a complication of gastric bypass surgery. Timely and effective management has important prognostic implications. This case highlights a minimally invasive endoscopic approach for GGF closure. The aim is to further discuss this technique as an alternative to surgical management of GGFs.
Case Description/Methods: A 53-year-old female with comorbid obesity and steatohepatitis presented for evaluation of worsening reflux following Roux-en-Y gastric bypass (RYGB) 14 years prior. Her RYGB was complicated by a leak at the gastrojejunal anastomosis, necessitating reoperation. The patient's reflux was unresponsive to esomeprazole 40 mg twice daily. Esophagogastroduodenoscopy (EGD) and esophagram identified a GGF, thought to be contributing to the patient’s symptoms.
Both gastroenterology and bariatric surgery teams assessed the patient, discussing endoscopic and surgical closure options. The patient favored an endoscopic approach due to the high risk of requiring conversion to esophagojejunostomy if the fistula was surgically addressed, given its location near the gastroesophageal junction.
The patient underwent endoscopic closure utilizing a mucosectomy technique with placement of an over-the-scope clip (OTSC) and two anchors, without complications (Figure 1 A-C). This technique was chosen to ensure muscle-to-muscle apposition and increase the chance of durable closure, given the limited space for endoscopic suturing. Intra-procedural contrast showed no signs of extravasation or remaining fistula tract when observed under fluoroscopy. At 4-month follow-up, the patient reported improvement in reflux symptoms. She is scheduled for repeat imaging and endoscopy to assess for sustained closure of the fistula.
Discussion: This case describes the successful use of endoscopic mucosectomy with OTSC clip placement for closure of a GGF in a patient with prior RYBG. This procedure offers a reasonable alternative for GGF closure, particularly when anatomical constraints limit the feasibility of endoscopic suturing. The patient preferred this minimally invasive approach due to the high risk of complications associated with surgical intervention. The patient had a positive clinical outcome and will be closely monitored for sustainability of the closure.

Figure: Figure 1. A) Gastrogastric fistula identified at the gastrojejunal anastomosis estimated to be 15 mm in diameter. B) Mucosectomy was performed around the gastrogastric fistula using a hybrid needle knife followed by argon plasma coagulation to ablate the exposed mucosal surfaces of the mucosectomy edges. C) Following mucosectomy, an over-the-scope clip was placed using two anchor devices to help approximate the tissue edges.
Disclosures:
Brent Gawey indicated no relevant financial relationships.
Khushboo Gala indicated no relevant financial relationships.
Mark Hanscom indicated no relevant financial relationships.
Barham Abu Dayyeh: Apollo Endosurgery – Consultant, Grant/Research Support. Aspire Bariatrics – Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Cairn Diagnostics – Grant/Research Support. DyaMx – Consultant. Endogastric Solutions – Speakers Bureau. Endo-TAGSS – Consultant. GI Dynamics – Grant/Research Support. Johnson and Johnson – Speakers Bureau. Medtronic – Grant/Research Support. Olympus – Speakers Bureau. Spatz Medical – Grant/Research Support. USGI Medical – Consultant, Grant/Research Support.
Brent J. Gawey, MD, MSc, Khushboo Gala, MBBS, Mark Hanscom, MD, Barham Abu Dayyeh, MD, MPH. P2326 - Clipping the Culprit: Management of a Gastrogastric Fistula Using Mucosectomy and an Over-the-Scope Clip, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
