Monday Poster Session
Category: Interventional Endoscopy
P2329 - Combined EUS-Guided Glue and Coil Therapy for Management of Rectal Varices in Decompensated Cirrhosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- KT
Kshitij Thakur, MD, MSc
University of Kentucky
Lexington, Kentucky
Presenting Author(s)
Kshitij Thakur, MD, MSc, Ujas Patel, MD, Amber Cloud, MD, Jeeva Jaganathan, MD, Samuel Mardini, MD, MBA, MPH
University of Kentucky, Lexington, KY
Introduction: Portal hypertension related to decompensated cirrhosis can manifest with several complications including esophageal and gastric varices and portal hypertensive gastropathy causing upper gastrointestinal (GI) bleeding. Bleeding rectal varices is a rare source of lower GI bleeding in patients with cirrhosis. Available treatment modalities for bleeding rectal varices include banding, sclerotherapy, transjugular intrahepatic portosystemic shunt, balloon-occluded retrograde transvenous obliteration, glue embolization, or combined glue and coil embolization. We present a case of lower GI variceal bleed managed with dual endoscopic ultrasound (EUS) guided coil and cyanoacrylate therapies.
Case Description/Methods: An 80-year-old female patient with decompensated methotrexate-related cirrhosis presented with hematochezia resulting in acute blood loss anemia. For continued drop in hemoglobin from her baseline on serial monitoring, she did require transfusion of two units of packed red blood cells for hemoglobin less than 7 during her stay. Patient was started on ceftriaxone for spontaneous bacterial peritonitis prophylaxis, octreotide, and pantoprazole drips. EGD (esophagogastroduodenoscopy) and colonoscopy were performed with no significant findings on EGD, but the colonoscopy showed large non-bleeding rectal varices and grade III internal hemorrhoids that prolapse with strain requiring manual replacement. No active bleeding was identified on procedures. The case was referred to our advanced gastroenterology group. EUS revealed two large varices in communication with smaller varices. A single Nester coil of 14 mm (length) x 12 mm (diameter) was injected in each of the larger varices. Successful deployment of the coil was followed by injection of cyanoacrylate. Decreased doppler flow in the variceal column was visualized on EUS. Pale discoloration on direct endoscopic view confirmed at least partial sclerosis following treatment. Subsequent endoscopy was required one week later for repeat variceal treatment with band ligation of smaller distal varices.
Discussion: A rare portal hypertension-related complication is a severe lower GI bleed from rectal varices in a cirrhotic patient. There is no consensus on the optimal management for obliteration of these varices. When the endoscopy yields large rectal varices ( >3 cm in diameter), successful embolization using coils to provide scaffolding for retaining cyanoacrylate glue within the variceal column can be an effective management strategy for hemostasis.

Disclosures:
Kshitij Thakur, MD, MSc, Ujas Patel, MD, Amber Cloud, MD, Jeeva Jaganathan, MD, Samuel Mardini, MD, MBA, MPH. P2329 - Combined EUS-Guided Glue and Coil Therapy for Management of Rectal Varices in Decompensated Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Kentucky, Lexington, KY
Introduction: Portal hypertension related to decompensated cirrhosis can manifest with several complications including esophageal and gastric varices and portal hypertensive gastropathy causing upper gastrointestinal (GI) bleeding. Bleeding rectal varices is a rare source of lower GI bleeding in patients with cirrhosis. Available treatment modalities for bleeding rectal varices include banding, sclerotherapy, transjugular intrahepatic portosystemic shunt, balloon-occluded retrograde transvenous obliteration, glue embolization, or combined glue and coil embolization. We present a case of lower GI variceal bleed managed with dual endoscopic ultrasound (EUS) guided coil and cyanoacrylate therapies.
Case Description/Methods: An 80-year-old female patient with decompensated methotrexate-related cirrhosis presented with hematochezia resulting in acute blood loss anemia. For continued drop in hemoglobin from her baseline on serial monitoring, she did require transfusion of two units of packed red blood cells for hemoglobin less than 7 during her stay. Patient was started on ceftriaxone for spontaneous bacterial peritonitis prophylaxis, octreotide, and pantoprazole drips. EGD (esophagogastroduodenoscopy) and colonoscopy were performed with no significant findings on EGD, but the colonoscopy showed large non-bleeding rectal varices and grade III internal hemorrhoids that prolapse with strain requiring manual replacement. No active bleeding was identified on procedures. The case was referred to our advanced gastroenterology group. EUS revealed two large varices in communication with smaller varices. A single Nester coil of 14 mm (length) x 12 mm (diameter) was injected in each of the larger varices. Successful deployment of the coil was followed by injection of cyanoacrylate. Decreased doppler flow in the variceal column was visualized on EUS. Pale discoloration on direct endoscopic view confirmed at least partial sclerosis following treatment. Subsequent endoscopy was required one week later for repeat variceal treatment with band ligation of smaller distal varices.
Discussion: A rare portal hypertension-related complication is a severe lower GI bleed from rectal varices in a cirrhotic patient. There is no consensus on the optimal management for obliteration of these varices. When the endoscopy yields large rectal varices ( >3 cm in diameter), successful embolization using coils to provide scaffolding for retaining cyanoacrylate glue within the variceal column can be an effective management strategy for hemostasis.

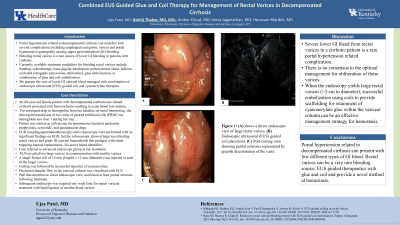
Figure: Figure 1: (A) shows a direct endoscopic view of large rectal varices. (B) Endoscopic ultrasound (EUS) guided coil placement. (C) Post-coiling view showing partial sclerosis represented by grayish discoloration of varix.
Disclosures:
Kshitij Thakur indicated no relevant financial relationships.
Ujas Patel indicated no relevant financial relationships.
Amber Cloud indicated no relevant financial relationships.
Jeeva Jaganathan indicated no relevant financial relationships.
Samuel Mardini indicated no relevant financial relationships.
Kshitij Thakur, MD, MSc, Ujas Patel, MD, Amber Cloud, MD, Jeeva Jaganathan, MD, Samuel Mardini, MD, MBA, MPH. P2329 - Combined EUS-Guided Glue and Coil Therapy for Management of Rectal Varices in Decompensated Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
