Monday Poster Session
Category: Liver
P2347 - Characterization of the Chronic Hepatitis B Care Cascade at a Large, Ethnically Diverse Veterans Affairs Cohort
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall

Shahrin Islam, BS, MS
David Geffen School of Medicine at University of California Los Angeles
Los Angeles, CA
Presenting Author(s)
Shahrin Islam, BS, MS1, Debika Bhattacharya, MD, MSc2, Arpan Patel, MD, PhD2
1David Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA; 2VA Greater Los Angeles Healthcare System, Los Angeles, CA
Introduction: Chronic hepatitis B (CHB) affects 9,670 Veterans, but care is associated with significant quality gaps, including delays in diagnosis & treatment initiation and access to specialty care. To guide system-level quality improvement (QI) initiatives to narrow these gaps, we aim to 1) characterize the Hepatitis B (HBV) care cascade & 2) describe factors associated with low-quality care at a VA that treats a large, diverse population.
Methods: We used the VA Advanced Liver Disease Dashboard to identify patients with CHB (history of two positive HbsAg tests 6 months apart or positive HBV DNA) from 1/1/96-5/1/2023 with chart review verification. Primary outcomes included: 1) receipt of full laboratory workup for HBV & 2) appropriate HBV treatment/non-treatment based on AASLD guidelines. We defined high-quality care as receipt of both measures. We abstracted sociodemographic (age, sex, race/ethnicity, history of housing insecurity, mental health disorder, or any substance use disorder and % service connection,) & clinical factors (linkage to specialty care, mention of CHB in primary care (PCP) documentation). To assess factors associated with low quality care, we used t-tests & Chi-squared tests, for continuous & categorical variables, respectively.
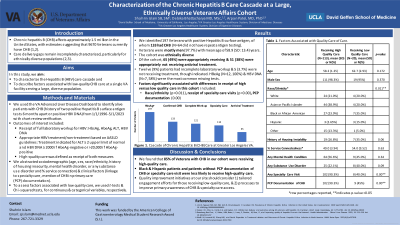
Results: We identified 197 Veterans, of whom 133 had CHB (N=64 did not repeat HpBsAg testing). Veterans were mostly men (97.7%) with a mean age of 58.9 (SD: 13.4) years. The cohort was ethnically diverse (Asian/Pacific Islander: 36%, Black/African American: 26%, Non-Hispanic White: 21%, Hispanic White: 4.5%, Other/Not Reporting: 13%). Of the cohort, 65 (49%) were appropriately receiving & 51 (38%) were appropriately not receiving antiviral treatment. Twelve (9%) patients had incomplete laboratory workup & five (3.7%) were not receiving treatment though indicated. HpBeAg (N=12, 100%) & HBV DNA (N=7, 58%) were the most common missing tests. Race/ethnicity (p=0.011), receipt of specialty care visits (p=0.00) & PCP documentation (0.00) were associated with differences in receipt of high versus low quality care (Table 1).
Discussion: We found that while 85% of Veterans with CHB in our cohort were receiving high-quality care, Black & Hispanic patients and patients without PCP documentation of CHB or specialty care visit were less likely to receive it. QI initiatives at our site should consider 1) tailored engagement efforts for those receiving low-quality care, & 2) processes to improve primary awareness of CHB & specialty care access.
Disclosures:
Shahrin Islam, BS, MS1, Debika Bhattacharya, MD, MSc2, Arpan Patel, MD, PhD2. P2347 - Characterization of the Chronic Hepatitis B Care Cascade at a Large, Ethnically Diverse Veterans Affairs Cohort, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1David Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA; 2VA Greater Los Angeles Healthcare System, Los Angeles, CA
Introduction: Chronic hepatitis B (CHB) affects 9,670 Veterans, but care is associated with significant quality gaps, including delays in diagnosis & treatment initiation and access to specialty care. To guide system-level quality improvement (QI) initiatives to narrow these gaps, we aim to 1) characterize the Hepatitis B (HBV) care cascade & 2) describe factors associated with low-quality care at a VA that treats a large, diverse population.
Methods: We used the VA Advanced Liver Disease Dashboard to identify patients with CHB (history of two positive HbsAg tests 6 months apart or positive HBV DNA) from 1/1/96-5/1/2023 with chart review verification. Primary outcomes included: 1) receipt of full laboratory workup for HBV & 2) appropriate HBV treatment/non-treatment based on AASLD guidelines. We defined high-quality care as receipt of both measures. We abstracted sociodemographic (age, sex, race/ethnicity, history of housing insecurity, mental health disorder, or any substance use disorder and % service connection,) & clinical factors (linkage to specialty care, mention of CHB in primary care (PCP) documentation). To assess factors associated with low quality care, we used t-tests & Chi-squared tests, for continuous & categorical variables, respectively.
Results: We identified 197 Veterans, of whom 133 had CHB (N=64 did not repeat HpBsAg testing). Veterans were mostly men (97.7%) with a mean age of 58.9 (SD: 13.4) years. The cohort was ethnically diverse (Asian/Pacific Islander: 36%, Black/African American: 26%, Non-Hispanic White: 21%, Hispanic White: 4.5%, Other/Not Reporting: 13%). Of the cohort, 65 (49%) were appropriately receiving & 51 (38%) were appropriately not receiving antiviral treatment. Twelve (9%) patients had incomplete laboratory workup & five (3.7%) were not receiving treatment though indicated. HpBeAg (N=12, 100%) & HBV DNA (N=7, 58%) were the most common missing tests. Race/ethnicity (p=0.011), receipt of specialty care visits (p=0.00) & PCP documentation (0.00) were associated with differences in receipt of high versus low quality care (Table 1).
Discussion: We found that while 85% of Veterans with CHB in our cohort were receiving high-quality care, Black & Hispanic patients and patients without PCP documentation of CHB or specialty care visit were less likely to receive it. QI initiatives at our site should consider 1) tailored engagement efforts for those receiving low-quality care, & 2) processes to improve primary awareness of CHB & specialty care access.
Disclosures:
Shahrin Islam indicated no relevant financial relationships.
Debika Bhattacharya: Gilead Sciences – Grant/Research Support.
Arpan Patel indicated no relevant financial relationships.
Shahrin Islam, BS, MS1, Debika Bhattacharya, MD, MSc2, Arpan Patel, MD, PhD2. P2347 - Characterization of the Chronic Hepatitis B Care Cascade at a Large, Ethnically Diverse Veterans Affairs Cohort, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
