Monday Poster Session
Category: Liver
P2349 - Rates and Adherence of Statin Use for Primary or Secondary Prevention of ASCVD in Liver Transplant Recipients
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Debra W. Yen, MD
University of Cincinnati Medical Center
Cincinnati, OH
Presenting Author(s)
Debra W. Yen, MD, Jacob A. Ciricillo, MD, Yeshika Sharma, MD, Askanda Osman, MD, Michael Clanahan, MD, Inuk Zandvakili, MD, PhD, Amoah Yeboah-Korang, MD, MPH
University of Cincinnati Medical Center, Cincinnati, OH
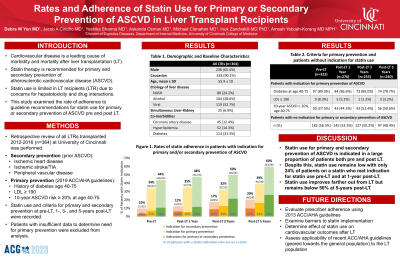
Introduction: Cardiovascular disease is a leading cause of morbidity and mortality after liver transplantation (LT), which highlights the importance of prevention and management of cardiac disease in the post-transplant setting. In the general population, statin therapy is recommended for primary and secondary prevention of atherosclerotic cardiovascular disease (ASCVD). However, statin use in LT recipients (LTR) remains limited due to concerns for hepatotoxicity and potential for drug interactions. This study aims to elucidate the proportion of patients who met indication for statin use for primary or secondary prevention of ASCVD pre and post LT based on 2019 ACC/AHA guidelines, as well as adherence to statins.
Methods: Retrospective review of all LTRs transplanted 2012-2016 at a single center was performed. Patients with prior ASCVD such as ischemic heart disease, ischemic stroke/TIA, and peripheral vascular disease met indication for secondary prevention. Indications for statin use for primary prevention included history of diabetes at age 40-75, LDL ≥ 190, and 10-year ASCVD risk ≥ 20% at age 40-75. Statin use and criteria for primary or secondary prevention at pre-LT and at 1-, 3- and 5-years post-LT were recorded. Patients with insufficient data to determine need for primary prevention were excluded from analysis.
Results: Among 364 LTRs, 65.4% were male and 90.1% Caucasian. Mean age was 55.9 ± 10 at LT, and 23.1% had NASH cirrhosis. Before LT, 12.4% had coronary artery disease, 14.3% hyperlipidemia, and 31.3% diabetes. Pre-LT, 9.6% met indication for secondary prevention of ASCVD (35.5% on statin), 33.9% met indications for primary prevention (21.1% on statin), and 43.5% met indications for either primary or secondary prevention (24.3% on statin) (Table 1). By 5 years post-LT, 20.4% met indication for secondary prevention (46.9% on statin), 39.2% met indications for primary prevention (41.5% on statin), and 59.6% met indications for either primary or secondary prevention (43.4% on statin).
Discussion: In this cohort, statin use for primary and secondary prevention of ASCVD is indicated in a large proportion of patients both pre and post-LT. However, prescriber adherence to guidelines remains low with only 24% of patients on a statin who met indication for statin use pre-LT and at 1 year post-LT. Adherence improves farther out from LT but remains below 50% at 5 years post-LT. Further exploration of barriers to statin implementation is needed.
Disclosures:
Debra W. Yen, MD, Jacob A. Ciricillo, MD, Yeshika Sharma, MD, Askanda Osman, MD, Michael Clanahan, MD, Inuk Zandvakili, MD, PhD, Amoah Yeboah-Korang, MD, MPH. P2349 - Rates and Adherence of Statin Use for Primary or Secondary Prevention of ASCVD in Liver Transplant Recipients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Cincinnati Medical Center, Cincinnati, OH
Introduction: Cardiovascular disease is a leading cause of morbidity and mortality after liver transplantation (LT), which highlights the importance of prevention and management of cardiac disease in the post-transplant setting. In the general population, statin therapy is recommended for primary and secondary prevention of atherosclerotic cardiovascular disease (ASCVD). However, statin use in LT recipients (LTR) remains limited due to concerns for hepatotoxicity and potential for drug interactions. This study aims to elucidate the proportion of patients who met indication for statin use for primary or secondary prevention of ASCVD pre and post LT based on 2019 ACC/AHA guidelines, as well as adherence to statins.
Methods: Retrospective review of all LTRs transplanted 2012-2016 at a single center was performed. Patients with prior ASCVD such as ischemic heart disease, ischemic stroke/TIA, and peripheral vascular disease met indication for secondary prevention. Indications for statin use for primary prevention included history of diabetes at age 40-75, LDL ≥ 190, and 10-year ASCVD risk ≥ 20% at age 40-75. Statin use and criteria for primary or secondary prevention at pre-LT and at 1-, 3- and 5-years post-LT were recorded. Patients with insufficient data to determine need for primary prevention were excluded from analysis.
Results: Among 364 LTRs, 65.4% were male and 90.1% Caucasian. Mean age was 55.9 ± 10 at LT, and 23.1% had NASH cirrhosis. Before LT, 12.4% had coronary artery disease, 14.3% hyperlipidemia, and 31.3% diabetes. Pre-LT, 9.6% met indication for secondary prevention of ASCVD (35.5% on statin), 33.9% met indications for primary prevention (21.1% on statin), and 43.5% met indications for either primary or secondary prevention (24.3% on statin) (Table 1). By 5 years post-LT, 20.4% met indication for secondary prevention (46.9% on statin), 39.2% met indications for primary prevention (41.5% on statin), and 59.6% met indications for either primary or secondary prevention (43.4% on statin).
Discussion: In this cohort, statin use for primary and secondary prevention of ASCVD is indicated in a large proportion of patients both pre and post-LT. However, prescriber adherence to guidelines remains low with only 24% of patients on a statin who met indication for statin use pre-LT and at 1 year post-LT. Adherence improves farther out from LT but remains below 50% at 5 years post-LT. Further exploration of barriers to statin implementation is needed.
Disclosures:
Debra Yen indicated no relevant financial relationships.
Jacob Ciricillo indicated no relevant financial relationships.
Yeshika Sharma indicated no relevant financial relationships.
Askanda Osman indicated no relevant financial relationships.
Michael Clanahan indicated no relevant financial relationships.
Inuk Zandvakili indicated no relevant financial relationships.
Amoah Yeboah-Korang indicated no relevant financial relationships.
Debra W. Yen, MD, Jacob A. Ciricillo, MD, Yeshika Sharma, MD, Askanda Osman, MD, Michael Clanahan, MD, Inuk Zandvakili, MD, PhD, Amoah Yeboah-Korang, MD, MPH. P2349 - Rates and Adherence of Statin Use for Primary or Secondary Prevention of ASCVD in Liver Transplant Recipients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
