Monday Poster Session
Category: Liver
P2363 - Serum Fibrosis and Steatosis Biomarkers for the Prediction of Mortality in Liver Transplant Recipients
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Thierry Fotsing Tadjo, BSc
Research Institute of McGill University Health Centre
Montreal, QC, Canada
Presenting Author(s)
Thierry Fotsing Tadjo, BSc, Alshaima Alhinai, MD, Marc Deschenes, MD, Philip Wong, MD, Tianyan Chen, MD, Frederic Lamonde, MD, Agnihotran V. Ramanakumar, MD, Nasim Saberi, MD, Jeffrey Barkun, MD, Giada Sebastiani, MD
Research Institute of McGill University Health Centre, Montreal, PQ, Canada
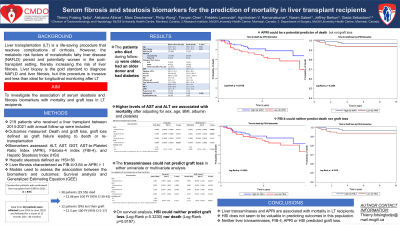
Introduction: Liver transplantation (LT) is a life-saving procedure that resolves complications of cirrhosis. However, the metabolic risk factors for nonalcoholic fatty liver disease (NAFLD) persist and potentially worsen in the post-transplant setting, thereby increasing the risk of liver fibrosis. Liver biopsy is the gold standard to diagnose NAFLD and liver fibrosis, but this procedure is invasive and less than ideal for longitudinal monitoring after LT. We aimed to investigate the association of serum steatosis and fibrosis biomarkers with mortality and graft loss in LT recipients.
Methods: We included consecutive adults who received a liver transplant at the MUHC in 2014-2021 and were followed up annually. The outcomes measured were death and graft loss, graft loss being defined as graft failure leading to death or re-transplantation. We assessed the prognostic value of the biomarkers ALT, AST, GGT, AST-to-Platelet Ratio Index (APRI), fibrosis-4 index (FIB-4), and hepatic steatosis index (HSI). Hepatic steatosis was defined as HSI >36, and liver fibrosis was characterized as FIB-4 > 3.64 or APRI > 1. Survival analysis and Generalized Estimating Equation (GEE) models were used to assess the association between the biomarkers and the outcomes.
Results: Two hundred nineteen patients were followed for 30 months on average. Graft loss and mortality occurred in 12 patients (9%) and 38 (29.5%) resulting in incidence rates of 29.5 (95% CI 20.9-40.6) and 9.6 (95% CI 5-16.8) per 100 person-years, respectively. Patients who died during the follow-up were older, had an older donor, and had a history of diabetes. On multivariable analysis using the GEE model (see Table), higher ALT and higher AST were associated with mortality after adjustment for sex, BMI, age, albumin, and platelets. In the time-to-event analysis, the Kaplan Meier curves showed that APRI >1 could be a potential predictor of mortality (P=0.0729 see Figure). Neither FIB-4 (log-rank, p = 0.199) nor HSI (log-rank, p = 0.919) were associated with mortality. None of the biomarkers or liver transaminases were associated with graft loss.
Discussion: Liver transaminases and the serum fibrosis biomarker APRI are associated with mortality in LT recipients. The hepatic steatosis biomarker HSI does not seem to be valuable in predicting outcomes in this population. None among liver transaminases, steatosis or fibrosis biomarkers predicted graft loss.

Disclosures:
Thierry Fotsing Tadjo, BSc, Alshaima Alhinai, MD, Marc Deschenes, MD, Philip Wong, MD, Tianyan Chen, MD, Frederic Lamonde, MD, Agnihotran V. Ramanakumar, MD, Nasim Saberi, MD, Jeffrey Barkun, MD, Giada Sebastiani, MD. P2363 - Serum Fibrosis and Steatosis Biomarkers for the Prediction of Mortality in Liver Transplant Recipients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Research Institute of McGill University Health Centre, Montreal, PQ, Canada
Introduction: Liver transplantation (LT) is a life-saving procedure that resolves complications of cirrhosis. However, the metabolic risk factors for nonalcoholic fatty liver disease (NAFLD) persist and potentially worsen in the post-transplant setting, thereby increasing the risk of liver fibrosis. Liver biopsy is the gold standard to diagnose NAFLD and liver fibrosis, but this procedure is invasive and less than ideal for longitudinal monitoring after LT. We aimed to investigate the association of serum steatosis and fibrosis biomarkers with mortality and graft loss in LT recipients.
Methods: We included consecutive adults who received a liver transplant at the MUHC in 2014-2021 and were followed up annually. The outcomes measured were death and graft loss, graft loss being defined as graft failure leading to death or re-transplantation. We assessed the prognostic value of the biomarkers ALT, AST, GGT, AST-to-Platelet Ratio Index (APRI), fibrosis-4 index (FIB-4), and hepatic steatosis index (HSI). Hepatic steatosis was defined as HSI >36, and liver fibrosis was characterized as FIB-4 > 3.64 or APRI > 1. Survival analysis and Generalized Estimating Equation (GEE) models were used to assess the association between the biomarkers and the outcomes.
Results: Two hundred nineteen patients were followed for 30 months on average. Graft loss and mortality occurred in 12 patients (9%) and 38 (29.5%) resulting in incidence rates of 29.5 (95% CI 20.9-40.6) and 9.6 (95% CI 5-16.8) per 100 person-years, respectively. Patients who died during the follow-up were older, had an older donor, and had a history of diabetes. On multivariable analysis using the GEE model (see Table), higher ALT and higher AST were associated with mortality after adjustment for sex, BMI, age, albumin, and platelets. In the time-to-event analysis, the Kaplan Meier curves showed that APRI >1 could be a potential predictor of mortality (P=0.0729 see Figure). Neither FIB-4 (log-rank, p = 0.199) nor HSI (log-rank, p = 0.919) were associated with mortality. None of the biomarkers or liver transaminases were associated with graft loss.
Discussion: Liver transaminases and the serum fibrosis biomarker APRI are associated with mortality in LT recipients. The hepatic steatosis biomarker HSI does not seem to be valuable in predicting outcomes in this population. None among liver transaminases, steatosis or fibrosis biomarkers predicted graft loss.

Figure: Figure. Kaplan-Meier survival curve in LT patients according to the APRI biomarker
Disclosures:
Thierry Fotsing Tadjo indicated no relevant financial relationships.
Alshaima Alhinai indicated no relevant financial relationships.
Marc Deschenes indicated no relevant financial relationships.
Philip Wong indicated no relevant financial relationships.
Tianyan Chen indicated no relevant financial relationships.
Frederic Lamonde indicated no relevant financial relationships.
Agnihotran V. Ramanakumar indicated no relevant financial relationships.
Nasim Saberi indicated no relevant financial relationships.
Jeffrey Barkun indicated no relevant financial relationships.
Giada Sebastiani indicated no relevant financial relationships.
Thierry Fotsing Tadjo, BSc, Alshaima Alhinai, MD, Marc Deschenes, MD, Philip Wong, MD, Tianyan Chen, MD, Frederic Lamonde, MD, Agnihotran V. Ramanakumar, MD, Nasim Saberi, MD, Jeffrey Barkun, MD, Giada Sebastiani, MD. P2363 - Serum Fibrosis and Steatosis Biomarkers for the Prediction of Mortality in Liver Transplant Recipients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
