Monday Poster Session
Category: Liver
P2365 - Role of Hepatobiliary Testing in Predicting In-Hospital Mortality From COVID-19
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Prithi Choday, MD
Hemet Global Medical Center
Hemet, CA
Presenting Author(s)
Prithi Choday, MD1, Chukwuemeka Umeh, MD, MPH1, Anphong Nguyen, MD1, Isha Samreen, MD1, Tri Ly, MD1, Sukhwinder Jhooty, BS2, Pranav Barve, MD, MPH1, Sumanta Chaudhuri, MD1, Sreenivasa Nakka, MD, FACG1
1Hemet Global Medical Center, Hemet, CA; 2American University of Antigua, Hemet, CA
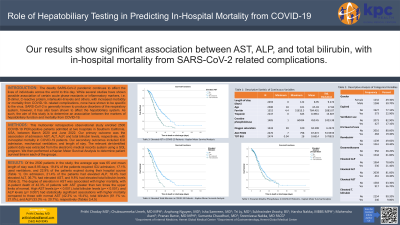
Introduction: The deadly SARS-CoV-2 pandemic continues to affect the lives of individuals across the world to this day. While several studies have shown possible association of certain acute phase reactants or inflammatory markers, i.e. D-dimer, C-reactive protein, interleukin-6 levels and others, with increased morbidity or mortality from COVID-19- related complications, none have shown to be specific to the virus. SARS-CoV-2 is generally known to produce disorders of the respiratory system, however, it has also been shown to affect the hepatobiliary system. As such, the aim of this study is to determine an association between the markers of hepatobiliary function and mortality from COVID-19.
Methods: This multicenter retrospective observational study enrolled 2500 COVID-19 PCR-positive patients admitted at two hospitals in Southern California, USA, between March 2020 and June 2022. Our primary outcome was the association of admission AST, ALT, ALP, and total bilirubin levels, respectively, with in-hospital mortality in COVID-19 patients. Our secondary outcomes included ICU admission, mechanical ventilation, and length of stay. The relevant de-identified patient data was extracted from the electronic medical records system using a SQL program. We then performed a Kaplan Meier Survival Analysis to determine patient survival time in each of the groups.
Results: Of the 2500 patients in the study, the average age was 65 and mean length of stay was 8.95 days. 19.4% of the patients required ICU admission, 17.1% used ventilators, and 22.9% of the patients expired during their hospital course (Table 1). On admission, 21.4% of the patients had elevated ALP, 18.4% had elevated ALT, 36.7% had elevated AST, and 9.8% had elevated total bilirubin levels. The degree of elevation in AST was associated with higher mortality, with in-patient death of 42.3% of patients with AST greater than two times the upper limits of normal. High AST levels (p= < 0.001), total bilirubin levels (p= < 0.001), and ALP levels (p= 0.007) had statistically significant associations with higher mortality compared to those with normal AST (42.3% vs 16.4%), total bilirubin (61.1% vs. 21.0%), and ALP (33.3% vs. 20.7%), respectively.
Discussion: Our results show significant association between AST, ALP, and total bilirubin, with in-hospital mortality from SARS-CoV-2 related complications. These results warrant further larger scale studies to determine use of hepatobiliary function testing in prediction of patient outcomes in COVID-19.

Disclosures:
Prithi Choday, MD1, Chukwuemeka Umeh, MD, MPH1, Anphong Nguyen, MD1, Isha Samreen, MD1, Tri Ly, MD1, Sukhwinder Jhooty, BS2, Pranav Barve, MD, MPH1, Sumanta Chaudhuri, MD1, Sreenivasa Nakka, MD, FACG1. P2365 - Role of Hepatobiliary Testing in Predicting In-Hospital Mortality From COVID-19, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Hemet Global Medical Center, Hemet, CA; 2American University of Antigua, Hemet, CA
Introduction: The deadly SARS-CoV-2 pandemic continues to affect the lives of individuals across the world to this day. While several studies have shown possible association of certain acute phase reactants or inflammatory markers, i.e. D-dimer, C-reactive protein, interleukin-6 levels and others, with increased morbidity or mortality from COVID-19- related complications, none have shown to be specific to the virus. SARS-CoV-2 is generally known to produce disorders of the respiratory system, however, it has also been shown to affect the hepatobiliary system. As such, the aim of this study is to determine an association between the markers of hepatobiliary function and mortality from COVID-19.
Methods: This multicenter retrospective observational study enrolled 2500 COVID-19 PCR-positive patients admitted at two hospitals in Southern California, USA, between March 2020 and June 2022. Our primary outcome was the association of admission AST, ALT, ALP, and total bilirubin levels, respectively, with in-hospital mortality in COVID-19 patients. Our secondary outcomes included ICU admission, mechanical ventilation, and length of stay. The relevant de-identified patient data was extracted from the electronic medical records system using a SQL program. We then performed a Kaplan Meier Survival Analysis to determine patient survival time in each of the groups.
Results: Of the 2500 patients in the study, the average age was 65 and mean length of stay was 8.95 days. 19.4% of the patients required ICU admission, 17.1% used ventilators, and 22.9% of the patients expired during their hospital course (Table 1). On admission, 21.4% of the patients had elevated ALP, 18.4% had elevated ALT, 36.7% had elevated AST, and 9.8% had elevated total bilirubin levels. The degree of elevation in AST was associated with higher mortality, with in-patient death of 42.3% of patients with AST greater than two times the upper limits of normal. High AST levels (p= < 0.001), total bilirubin levels (p= < 0.001), and ALP levels (p= 0.007) had statistically significant associations with higher mortality compared to those with normal AST (42.3% vs 16.4%), total bilirubin (61.1% vs. 21.0%), and ALP (33.3% vs. 20.7%), respectively.
Discussion: Our results show significant association between AST, ALP, and total bilirubin, with in-hospital mortality from SARS-CoV-2 related complications. These results warrant further larger scale studies to determine use of hepatobiliary function testing in prediction of patient outcomes in COVID-19.

Figure: Survival Functions in COVID-19 Patients with Elevated AST, Total Bilirubin, and Alkaline Phosphatase Levels
Disclosures:
Prithi Choday indicated no relevant financial relationships.
Chukwuemeka Umeh indicated no relevant financial relationships.
Anphong Nguyen indicated no relevant financial relationships.
Isha Samreen indicated no relevant financial relationships.
Tri Ly indicated no relevant financial relationships.
Sukhwinder Jhooty indicated no relevant financial relationships.
Pranav Barve indicated no relevant financial relationships.
Sumanta Chaudhuri indicated no relevant financial relationships.
Sreenivasa Nakka indicated no relevant financial relationships.
Prithi Choday, MD1, Chukwuemeka Umeh, MD, MPH1, Anphong Nguyen, MD1, Isha Samreen, MD1, Tri Ly, MD1, Sukhwinder Jhooty, BS2, Pranav Barve, MD, MPH1, Sumanta Chaudhuri, MD1, Sreenivasa Nakka, MD, FACG1. P2365 - Role of Hepatobiliary Testing in Predicting In-Hospital Mortality From COVID-19, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
