Monday Poster Session
Category: Liver
P2371 - Impact of Venous Thromboembolism During Admission for Alcoholic Hepatitis: A Retrospective Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

James Love, MD
University of Illinois at Chicago
Chicago, IL
Presenting Author(s)
James Love, MD1, Michael Siegel, DO1, Khaled Elfert, MD2, Elie Ghoulam, MD1, Ahmad Al-Taee, MD3, Asim Shuja, MD4
1University of Illinois at Chicago, Chicago, IL; 2SBH Health System, Bronx, NY; 3University of Illinois at Urbana–Champaign, Champaign, IL; 4University of Illinois Chicago, Chicago, IL
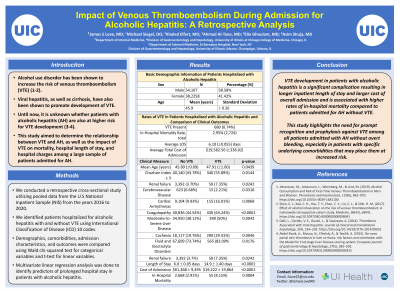
Introduction: Alcohol use disorder has been shown to increase the risk of venous thromboembolism (VTE). Viral hepatitis, as well as cirrhosis, have also been shown to promote development of VTE. It is unknown whether patients with alcoholic hepatitis (AH) are also at higher risk for VTE development. This study aims to determine the relationship between VTE and AH, as well as the impact of VTE on mortality, hospital length of stay (LOS), and hospital charges among a large sample of patients admitted for AH.
Methods: We conducted a retrospective cross-sectional study utilizing the U.S National Inpatient Sample (NIS) database from the years 2016-2020. We identified patients hospitalized for AH with and without VTE using International Classification of Disease (ICD) 10 codes. Demographics, comorbidities, admission characteristics, and outcomes were compared using Wald chi-squared test for categorical variables and t-test for linear variables. Multivariate linear regression analysis was done to identify predictors of prolonged hospital stay in patients with alcoholic hepatitis.
Results: Of the 92,365 adult patients admitted for AH, 680 patients experienced VTE. Patients who experienced VTE were slightly older (47.9+/-1.0 vs 45.9 +/- 0.1; p=0.044) and had higher Charlson Comorbidity Index (CCI) scores (CCI≥3 55.9% vs 43.8%; p=0.014). Specifically, patients with concurrent cerebrovascular disease, renal failure, cardiac arrhythmias, coagulopathy, moderate or severe liver disease, and cachexia developed VTE at higher rates compared to other comorbidities. In-hospital mortality rate was higher among patients with alcoholic hepatitis with concurrent VTE (8.15% vs 2.91%, p=0.0004), as was total LOS (14.9+/-1.40 vs 6.0 +/-0.05; p< 0.0001) and cost of admission ($61,368 +/-9495 vs $19,222 +/- 19864; p< 0.0001). The multivariate linear regression analysis showed that VTE was associated with an increase of 7.23 days in the mean LOS among patients admitted with alcoholic hepatitis (CI 4.61-9.85, p< 0.0001).
Discussion: VTE development in patients with alcoholic hepatitis is a significant complication resulting in longer inpatient LOS and larger cost of overall admission, and is associated with higher rates of in-hospital mortality compared to patients admitted for AH without VTE. This study highlights the need for prompt recognition and prophylaxis against VTE among all patients admitted with AH without overt bleeding, especially in patients with specific underlying comorbidities that may place them at increased risk.
Disclosures:
James Love, MD1, Michael Siegel, DO1, Khaled Elfert, MD2, Elie Ghoulam, MD1, Ahmad Al-Taee, MD3, Asim Shuja, MD4. P2371 - Impact of Venous Thromboembolism During Admission for Alcoholic Hepatitis: A Retrospective Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Illinois at Chicago, Chicago, IL; 2SBH Health System, Bronx, NY; 3University of Illinois at Urbana–Champaign, Champaign, IL; 4University of Illinois Chicago, Chicago, IL
Introduction: Alcohol use disorder has been shown to increase the risk of venous thromboembolism (VTE). Viral hepatitis, as well as cirrhosis, have also been shown to promote development of VTE. It is unknown whether patients with alcoholic hepatitis (AH) are also at higher risk for VTE development. This study aims to determine the relationship between VTE and AH, as well as the impact of VTE on mortality, hospital length of stay (LOS), and hospital charges among a large sample of patients admitted for AH.
Methods: We conducted a retrospective cross-sectional study utilizing the U.S National Inpatient Sample (NIS) database from the years 2016-2020. We identified patients hospitalized for AH with and without VTE using International Classification of Disease (ICD) 10 codes. Demographics, comorbidities, admission characteristics, and outcomes were compared using Wald chi-squared test for categorical variables and t-test for linear variables. Multivariate linear regression analysis was done to identify predictors of prolonged hospital stay in patients with alcoholic hepatitis.
Results: Of the 92,365 adult patients admitted for AH, 680 patients experienced VTE. Patients who experienced VTE were slightly older (47.9+/-1.0 vs 45.9 +/- 0.1; p=0.044) and had higher Charlson Comorbidity Index (CCI) scores (CCI≥3 55.9% vs 43.8%; p=0.014). Specifically, patients with concurrent cerebrovascular disease, renal failure, cardiac arrhythmias, coagulopathy, moderate or severe liver disease, and cachexia developed VTE at higher rates compared to other comorbidities. In-hospital mortality rate was higher among patients with alcoholic hepatitis with concurrent VTE (8.15% vs 2.91%, p=0.0004), as was total LOS (14.9+/-1.40 vs 6.0 +/-0.05; p< 0.0001) and cost of admission ($61,368 +/-9495 vs $19,222 +/- 19864; p< 0.0001). The multivariate linear regression analysis showed that VTE was associated with an increase of 7.23 days in the mean LOS among patients admitted with alcoholic hepatitis (CI 4.61-9.85, p< 0.0001).
Discussion: VTE development in patients with alcoholic hepatitis is a significant complication resulting in longer inpatient LOS and larger cost of overall admission, and is associated with higher rates of in-hospital mortality compared to patients admitted for AH without VTE. This study highlights the need for prompt recognition and prophylaxis against VTE among all patients admitted with AH without overt bleeding, especially in patients with specific underlying comorbidities that may place them at increased risk.
Disclosures:
James Love indicated no relevant financial relationships.
Michael Siegel indicated no relevant financial relationships.
Khaled Elfert indicated no relevant financial relationships.
Elie Ghoulam indicated no relevant financial relationships.
Ahmad Al-Taee indicated no relevant financial relationships.
Asim Shuja indicated no relevant financial relationships.
James Love, MD1, Michael Siegel, DO1, Khaled Elfert, MD2, Elie Ghoulam, MD1, Ahmad Al-Taee, MD3, Asim Shuja, MD4. P2371 - Impact of Venous Thromboembolism During Admission for Alcoholic Hepatitis: A Retrospective Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
