Monday Poster Session
Category: Liver
P2392 - The Effect of Co-Morbid Illness on Post-Transplant Survival in Patients with PSC from 2012-2021
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Nuval Cherian, MD
MedStar Washington Hospital Center
Washington, District of Columbia
Presenting Author(s)
Nuval Cherian, MD1, Esha Parikh, DO2
1MedStar Washington Hospital Center, Washington, DC; 2MedStar Georgetown University Hospital, Washington, DC
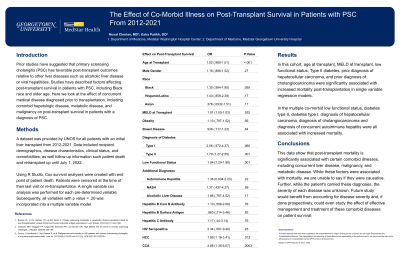
Introduction: Prior studies have suggested that primary sclerosing cholangitis (PSC) has favorable post-transplant outcomes relative to other liver diseases such as alcoholic liver disease or viral hepatitides. Studies have described factors affecting post-transplant survival in patients with PSC, including Black race and older age. Here we look at the effect of concurrent medical disease diagnosed prior to transplantation, including comorbid hepatologic disease, metabolic disease, and malignancy on post-transplant survival in patients with a diagnosis of PSC.
Methods: A dataset was provided by UNOS for all patients with an initial liver transplant from 2012-2021. Data included recipient demographics, disease characteristics, clinical status, and comorbidities, as well follow up information such patient death and retransplant up until July 1, 2022.
Using R Studio, Cox survival analyses were created with end point of patient death. Patients were censored at the time of their last visit or re-transplantation. A single variable cox analysis was performed for each pre-determined variable. Subsequently, all variables with p value < .20 was incorporated into a multiple variable model.
Results: In this cohort, age at transplant, MELD at transplant, low functional status, Type II diabetes, prior diagnosis of hepatocellular carcinoma, and prior diagnosis of cholangiocarcinoma were significantly associated with increased mortality post-transplantation in single variable regression models.
In the multiple co-morbid low functional status, diabetes type II, diabetes type I, diagnosis of hepatocellular carcinoma, diagnosis of cholangiocarcinoma and diagnosis of concurrent autoimmune hepatitis were all associated with increased mortality.
Discussion: This data show that post-transplant mortality is significantly associated with certain comorbid illnesses, including concurrent liver disease, malignancy, and metabolic disease. While these factors were associated with mortality, we are unable to say if they were causative. Further, while the patient's carried these diagnoses, the severity of each disease was unknown. Future study would benefit from accounting for disease severity and, if done prospectively, could even study the effect of effective management and treatment of these comorbid diseases on patient survival.
Disclosures:
Nuval Cherian, MD1, Esha Parikh, DO2. P2392 - The Effect of Co-Morbid Illness on Post-Transplant Survival in Patients with PSC from 2012-2021, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1MedStar Washington Hospital Center, Washington, DC; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Prior studies have suggested that primary sclerosing cholangitis (PSC) has favorable post-transplant outcomes relative to other liver diseases such as alcoholic liver disease or viral hepatitides. Studies have described factors affecting post-transplant survival in patients with PSC, including Black race and older age. Here we look at the effect of concurrent medical disease diagnosed prior to transplantation, including comorbid hepatologic disease, metabolic disease, and malignancy on post-transplant survival in patients with a diagnosis of PSC.
Methods: A dataset was provided by UNOS for all patients with an initial liver transplant from 2012-2021. Data included recipient demographics, disease characteristics, clinical status, and comorbidities, as well follow up information such patient death and retransplant up until July 1, 2022.
Using R Studio, Cox survival analyses were created with end point of patient death. Patients were censored at the time of their last visit or re-transplantation. A single variable cox analysis was performed for each pre-determined variable. Subsequently, all variables with p value < .20 was incorporated into a multiple variable model.
Results: In this cohort, age at transplant, MELD at transplant, low functional status, Type II diabetes, prior diagnosis of hepatocellular carcinoma, and prior diagnosis of cholangiocarcinoma were significantly associated with increased mortality post-transplantation in single variable regression models.
In the multiple co-morbid low functional status, diabetes type II, diabetes type I, diagnosis of hepatocellular carcinoma, diagnosis of cholangiocarcinoma and diagnosis of concurrent autoimmune hepatitis were all associated with increased mortality.
Discussion: This data show that post-transplant mortality is significantly associated with certain comorbid illnesses, including concurrent liver disease, malignancy, and metabolic disease. While these factors were associated with mortality, we are unable to say if they were causative. Further, while the patient's carried these diagnoses, the severity of each disease was unknown. Future study would benefit from accounting for disease severity and, if done prospectively, could even study the effect of effective management and treatment of these comorbid diseases on patient survival.
Disclosures:
Nuval Cherian indicated no relevant financial relationships.
Esha Parikh indicated no relevant financial relationships.
Nuval Cherian, MD1, Esha Parikh, DO2. P2392 - The Effect of Co-Morbid Illness on Post-Transplant Survival in Patients with PSC from 2012-2021, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
