Monday Poster Session
Category: Liver
P2410 - Barriers and Facilitators of Palliative Care Referrals for Patients with Cirrhosis: A Qualitative Study of Clinical Perspectives
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- KT
Kshitij Thakur, MD, MSc
University of Kentucky
Lexington, Kentucky
Presenting Author(s)
Kshitij Thakur, MD, MSc, Alla Grigorian, MD, PhD, Jessica McFarlin, MD, Allison Merritt, MPH, Jerod Stapleton, PhD
University of Kentucky, Lexington, KY
Introduction: Patients with cirrhosis develop debilitating symptoms and complications like hepatic encephalopathy, variceal bleeding, and ascites as the disease progresses. These patients often suffer from poor health-related quality of life and debilitating symptoms like pain, fatigue, confusion, muscle wasting, and perception of disability. Palliative care reduces healthcare costs and improves the quality of care and communication between patients/families and their providers in oncology settings. Cirrhosis patients rarely receive palliative care despite having a symptom burden similar to oncology patients. This study aims to identify barriers and facilitators of palliative care referral for patients with cirrhosis from the perspective of the hepatologists and gastroenterologists
Methods: The cross-sectional qualitative design included semi structured interviews (N=10, median duration-38 minutes) with hepatologist and gastroenterologist at our tertiary care academic center. These participants were selected using purposeful sampling. We developed an interview guide based on the literature review and our prior research. All interviews were audio recorded and transcribed verbatim. The Framework Method of Data Analysis(Gale, 2013) was used. Interviews were analyzed using a codebook by two investigators until both agreed that thematic saturation has reached
Results: The data reveals seven categories of barriers and facilitators of palliative care referral for patients with cirrhosis. Barriers include (1) Misconception about the scope of care provided by palliative care providers, (2) lack of access to outpatient palliative care, (3) adverse impact of palliative Care consultation on transplant listing, and (4) lack of operational pathways to assess unmet palliative care needs. Facilitated included (1) more clinician and patient education on the role and scope of palliative Care, (2) embedded palliative care in the hepatology clinic, and (3) a multidisciplinary team approach to palliative care can address multiple patient concerns, including caregiver burnout.
Discussion: Participants described why providers do not refer patients with cirrhosis to palliative care. The study highlights that there are both physician and institutional-level barriers to implementing a solid palliative hepatology program. This information can help guide future implementation studies to incorporate Palliative Care into cirrhosis management.

Disclosures:
Kshitij Thakur, MD, MSc, Alla Grigorian, MD, PhD, Jessica McFarlin, MD, Allison Merritt, MPH, Jerod Stapleton, PhD. P2410 - Barriers and Facilitators of Palliative Care Referrals for Patients with Cirrhosis: A Qualitative Study of Clinical Perspectives, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Kentucky, Lexington, KY
Introduction: Patients with cirrhosis develop debilitating symptoms and complications like hepatic encephalopathy, variceal bleeding, and ascites as the disease progresses. These patients often suffer from poor health-related quality of life and debilitating symptoms like pain, fatigue, confusion, muscle wasting, and perception of disability. Palliative care reduces healthcare costs and improves the quality of care and communication between patients/families and their providers in oncology settings. Cirrhosis patients rarely receive palliative care despite having a symptom burden similar to oncology patients. This study aims to identify barriers and facilitators of palliative care referral for patients with cirrhosis from the perspective of the hepatologists and gastroenterologists
Methods: The cross-sectional qualitative design included semi structured interviews (N=10, median duration-38 minutes) with hepatologist and gastroenterologist at our tertiary care academic center. These participants were selected using purposeful sampling. We developed an interview guide based on the literature review and our prior research. All interviews were audio recorded and transcribed verbatim. The Framework Method of Data Analysis(Gale, 2013) was used. Interviews were analyzed using a codebook by two investigators until both agreed that thematic saturation has reached
Results: The data reveals seven categories of barriers and facilitators of palliative care referral for patients with cirrhosis. Barriers include (1) Misconception about the scope of care provided by palliative care providers, (2) lack of access to outpatient palliative care, (3) adverse impact of palliative Care consultation on transplant listing, and (4) lack of operational pathways to assess unmet palliative care needs. Facilitated included (1) more clinician and patient education on the role and scope of palliative Care, (2) embedded palliative care in the hepatology clinic, and (3) a multidisciplinary team approach to palliative care can address multiple patient concerns, including caregiver burnout.
Discussion: Participants described why providers do not refer patients with cirrhosis to palliative care. The study highlights that there are both physician and institutional-level barriers to implementing a solid palliative hepatology program. This information can help guide future implementation studies to incorporate Palliative Care into cirrhosis management.

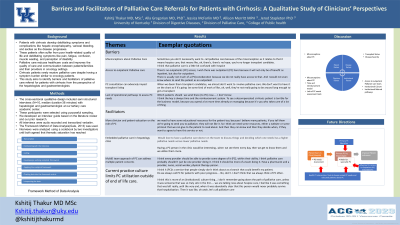
Figure: Visual Abstract
Disclosures:
Kshitij Thakur indicated no relevant financial relationships.
Alla Grigorian indicated no relevant financial relationships.
Jessica McFarlin indicated no relevant financial relationships.
Allison Merritt indicated no relevant financial relationships.
Jerod Stapleton indicated no relevant financial relationships.
Kshitij Thakur, MD, MSc, Alla Grigorian, MD, PhD, Jessica McFarlin, MD, Allison Merritt, MPH, Jerod Stapleton, PhD. P2410 - Barriers and Facilitators of Palliative Care Referrals for Patients with Cirrhosis: A Qualitative Study of Clinical Perspectives, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
