Monday Poster Session
Category: Liver
P2412 - Racial Differences in Cirrhosis Etiology and Manifestation in a Predominately African American Urban Medical Center
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Aabid M. Mohiuddin, DO
Detroit Medical Center/Wayne State University
Detroit, MI
Presenting Author(s)
Aabid Mohiuddin, DO1, Jasdeep Bathla, DO2, Ahmad Alnasarat, MD3, Astha Saini, MD3, Anirudh R. Damughatla, DO2, Mohamad Khaled Almujarkesh, MD3, Vanessa Milan-Ortiz, MD2, GokTurk Tepe, BS3, Paul H. Naylor, PhD3, Milton G. Mutchnick, MD3, Paul Kim, BS3
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 3Wayne State University School of Medicine, Detroit, MI
Introduction: While national trends reflect a decline in HCV related cirrhosis, hepatocellular carcinoma, and liver transplant, it remains critical to evaluate local trends in urban university medical centers with respect to African American (AA) individuals as compared to non-AA individuals. The objective of this study was to evaluate cirrhosis in AA as compared to non-AA individuals.
Methods: Using ICD-10 codes, we identified individuals with cirrhosis seen in a predominately AA urban university medical center in the first six months of 2016. The accuracy for the diagnosis of cirrhosis was determined by reviewing the medical records for laboratory values (ALT/AST/Platelets/Albumin/Fibrospect), FibroScan, US/CT imaging, varices on EGD and signs of decompensation (ascites, encephalopathy and bleeding/banded varices). An accurate diagnosis of cirrhosis was determined for 198 patients (146 AA and 52 non-AA).
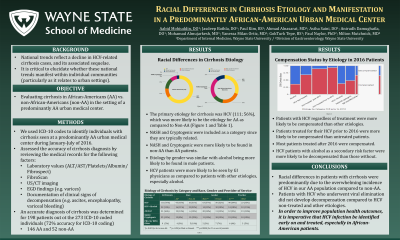
Results: The primary etiology for cirrhosis was HCV (111; 56%), followed by Alcohol (31) and HCV plus alcohol (22) (Table 1). NASH and Cryptogenic were included as a category since they are typically related. All other causes of liver disease (HBV, PBC, autoimmune hepatitis) were included in the other category. While etiology by gender was similar, AA were more likely to have HCV than non-AA. HCV patients were more likely to be seen by GI physicians as compared to patients with other etiologies, especially alcohol. With respect to decompensation at the time of 2016 assessment, patients with HCV were more likely to be compensated than other etiologies (Figure 1). This was also reflected by AA being more likely to be compensated than non-AA, due to the prevalence of HCV as the primary etiology of their cirrhosis. This protection from decompensation was likely due to the fact that if HCV patients had been treated and achieved an SVR, they were more likely to be compensated as compared to not treated patients (73% vs 20% ; p=0.0003)
Discussion: Racial differences in cirrhotic individuals were predominately due to the overwhelming incidence of HCV in our AA cirrhotic patients compared to non-AA. As a result of viral elimination in HCV individuals, they did not develop decompensation compared to HCV non-treated and other etiologies. Based on these observations, it is imperative that especially in AA patients HCV infection be identified and treated to improve health outcomes.

Disclosures:
Aabid Mohiuddin, DO1, Jasdeep Bathla, DO2, Ahmad Alnasarat, MD3, Astha Saini, MD3, Anirudh R. Damughatla, DO2, Mohamad Khaled Almujarkesh, MD3, Vanessa Milan-Ortiz, MD2, GokTurk Tepe, BS3, Paul H. Naylor, PhD3, Milton G. Mutchnick, MD3, Paul Kim, BS3. P2412 - Racial Differences in Cirrhosis Etiology and Manifestation in a Predominately African American Urban Medical Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 3Wayne State University School of Medicine, Detroit, MI
Introduction: While national trends reflect a decline in HCV related cirrhosis, hepatocellular carcinoma, and liver transplant, it remains critical to evaluate local trends in urban university medical centers with respect to African American (AA) individuals as compared to non-AA individuals. The objective of this study was to evaluate cirrhosis in AA as compared to non-AA individuals.
Methods: Using ICD-10 codes, we identified individuals with cirrhosis seen in a predominately AA urban university medical center in the first six months of 2016. The accuracy for the diagnosis of cirrhosis was determined by reviewing the medical records for laboratory values (ALT/AST/Platelets/Albumin/Fibrospect), FibroScan, US/CT imaging, varices on EGD and signs of decompensation (ascites, encephalopathy and bleeding/banded varices). An accurate diagnosis of cirrhosis was determined for 198 patients (146 AA and 52 non-AA).
Results: The primary etiology for cirrhosis was HCV (111; 56%), followed by Alcohol (31) and HCV plus alcohol (22) (Table 1). NASH and Cryptogenic were included as a category since they are typically related. All other causes of liver disease (HBV, PBC, autoimmune hepatitis) were included in the other category. While etiology by gender was similar, AA were more likely to have HCV than non-AA. HCV patients were more likely to be seen by GI physicians as compared to patients with other etiologies, especially alcohol. With respect to decompensation at the time of 2016 assessment, patients with HCV were more likely to be compensated than other etiologies (Figure 1). This was also reflected by AA being more likely to be compensated than non-AA, due to the prevalence of HCV as the primary etiology of their cirrhosis. This protection from decompensation was likely due to the fact that if HCV patients had been treated and achieved an SVR, they were more likely to be compensated as compared to not treated patients (73% vs 20% ; p=0.0003)
Discussion: Racial differences in cirrhotic individuals were predominately due to the overwhelming incidence of HCV in our AA cirrhotic patients compared to non-AA. As a result of viral elimination in HCV individuals, they did not develop decompensation compared to HCV non-treated and other etiologies. Based on these observations, it is imperative that especially in AA patients HCV infection be identified and treated to improve health outcomes.

Figure: Figure 1. The etiology of compensated and decompensated cirrhosis. The width of the bars represents the number of patients of each etiology and the height of the bar the ratio between compensated and decompensated cirrhotic individuals. NASH and Cryptogenic were included as a category since they are typically related. All other causes of liver disease (HBV, PBC, autoimmune hepatitis) were included in the other category
Disclosures:
Aabid Mohiuddin indicated no relevant financial relationships.
Jasdeep Bathla indicated no relevant financial relationships.
Ahmad Alnasarat indicated no relevant financial relationships.
Astha Saini indicated no relevant financial relationships.
Anirudh R. Damughatla indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Vanessa Milan-Ortiz indicated no relevant financial relationships.
GokTurk Tepe indicated no relevant financial relationships.
Paul Naylor: Janssen Biotech Inc – Grant/Research Support.
Milton Mutchnick: Chronic Liver Disease Foundation – Speakers Bureau. Janssen Biotech Inc – Grant/Research Support.
Paul Kim indicated no relevant financial relationships.
Aabid Mohiuddin, DO1, Jasdeep Bathla, DO2, Ahmad Alnasarat, MD3, Astha Saini, MD3, Anirudh R. Damughatla, DO2, Mohamad Khaled Almujarkesh, MD3, Vanessa Milan-Ortiz, MD2, GokTurk Tepe, BS3, Paul H. Naylor, PhD3, Milton G. Mutchnick, MD3, Paul Kim, BS3. P2412 - Racial Differences in Cirrhosis Etiology and Manifestation in a Predominately African American Urban Medical Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
