Monday Poster Session
Category: Liver
P2414 - Characterizing Practice Variations in the Care of Hospitalized Patients With Cirrhosis Across the University of California Health
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Jin Ge, MD, MBA
UCSF
San Francisco, CA
Presenting Author(s)
Jin Ge, MD, MBA1, Albert Lee, BA1, Oksana Gologorskaya, BS, MS1, Chiung-Yu Huang, PhD1, Mark J.. Pletcher, MD, MPH1, Jennifer C.. Lai, MD, MBA2
1UCSF, San Francisco, CA; 2University of California San Francisco, San Francisco, CA
Introduction: Despite publicly available practice guidelines published by AASLD and AGA, cirrhosis care remains highly variable. Investigating variations in guidelines-adherence could identify key opportunities to improve clinical outcomes, but prior studies have been limited by the lack of patient-level data. We aimed to overcome these limitations by leveraging a novel multicenter EHR database, the University of California Health Data Warehouse (UCHDW), with high-dimensional patient-level data to quantify adherence to national guidelines for inpatient cirrhosis care.
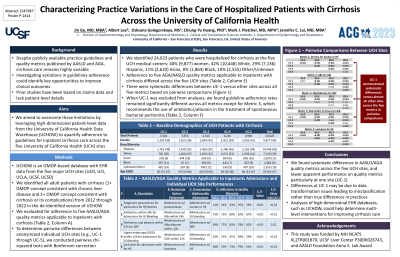
Methods: UCHDW is an Observational Model Outcomes Partnership (OMOP)-based database with EHR data from the five major medical centers of the University of California Health System (UCH). We identified all adult patients with cirrhosis (based on 1+ concept for chronic liver disease and 1+ concept for cirrhosis or its complications) from 2012 through 2022 in the de-identified version of UCHDW. We evaluated for adherence to five AASLD/AGA quality metrics applicable to inpatients with cirrhosis (Table 1, Column A). To determine pairwise differences between individual UCH sites, we conducted pairwise chi-squared tests with Bonferroni correction.
Results: We identified 24,628 patients who were hospitalized for cirrhosis or its complications at the five UC Health medical centers. The patient population was gender and racially/ethnically diverse: 40% women, 42% White, 29% Hispanic, 11% Asian, 8% Black, and 10% Other/Unknown. Median (IQR) age was 59 years (IQR 50-67). Adherence to five quality metrics applicable to inpatients with cirrhosis differed significantly between the five UCH sites (Table 1, Column E, p< 0.01 for all comparisons). In pairwise comparisons between individual UCH sites (e.g., UC-3 versus UC-5), we found systematic differences between UC-1 versus other sites across all five metrics. When UC-1 is excluded from analyses, we found guideline-adherence rates remained significantly different across all metrics except for Metric 3, which recommends the use of antibiotics/albumin in the treatment of spontaneous bacterial peritonitis (Table 1, Column F).
Discussion: We found systematic differences in AASLD/AGA quality metrics across the five UC Health medical centers, and lower apparent quality particularly at one site (UC-1), indicating specific opportunities for improvement. Analyses of high-dimensional EHR data, such as UCHDW, will enable comprehensive evaluations of multi-level factors for potential interventions in the future.
Disclosures:
Jin Ge, MD, MBA1, Albert Lee, BA1, Oksana Gologorskaya, BS, MS1, Chiung-Yu Huang, PhD1, Mark J.. Pletcher, MD, MPH1, Jennifer C.. Lai, MD, MBA2. P2414 - Characterizing Practice Variations in the Care of Hospitalized Patients With Cirrhosis Across the University of California Health, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UCSF, San Francisco, CA; 2University of California San Francisco, San Francisco, CA
Introduction: Despite publicly available practice guidelines published by AASLD and AGA, cirrhosis care remains highly variable. Investigating variations in guidelines-adherence could identify key opportunities to improve clinical outcomes, but prior studies have been limited by the lack of patient-level data. We aimed to overcome these limitations by leveraging a novel multicenter EHR database, the University of California Health Data Warehouse (UCHDW), with high-dimensional patient-level data to quantify adherence to national guidelines for inpatient cirrhosis care.
Methods: UCHDW is an Observational Model Outcomes Partnership (OMOP)-based database with EHR data from the five major medical centers of the University of California Health System (UCH). We identified all adult patients with cirrhosis (based on 1+ concept for chronic liver disease and 1+ concept for cirrhosis or its complications) from 2012 through 2022 in the de-identified version of UCHDW. We evaluated for adherence to five AASLD/AGA quality metrics applicable to inpatients with cirrhosis (Table 1, Column A). To determine pairwise differences between individual UCH sites, we conducted pairwise chi-squared tests with Bonferroni correction.
Results: We identified 24,628 patients who were hospitalized for cirrhosis or its complications at the five UC Health medical centers. The patient population was gender and racially/ethnically diverse: 40% women, 42% White, 29% Hispanic, 11% Asian, 8% Black, and 10% Other/Unknown. Median (IQR) age was 59 years (IQR 50-67). Adherence to five quality metrics applicable to inpatients with cirrhosis differed significantly between the five UCH sites (Table 1, Column E, p< 0.01 for all comparisons). In pairwise comparisons between individual UCH sites (e.g., UC-3 versus UC-5), we found systematic differences between UC-1 versus other sites across all five metrics. When UC-1 is excluded from analyses, we found guideline-adherence rates remained significantly different across all metrics except for Metric 3, which recommends the use of antibiotics/albumin in the treatment of spontaneous bacterial peritonitis (Table 1, Column F).
Discussion: We found systematic differences in AASLD/AGA quality metrics across the five UC Health medical centers, and lower apparent quality particularly at one site (UC-1), indicating specific opportunities for improvement. Analyses of high-dimensional EHR data, such as UCHDW, will enable comprehensive evaluations of multi-level factors for potential interventions in the future.
Disclosures:
Jin Ge: Astellas Pharmaceuticals – Consultant. Merck – Grant/Research Support.
Albert Lee indicated no relevant financial relationships.
Oksana Gologorskaya indicated no relevant financial relationships.
Chiung-Yu Huang indicated no relevant financial relationships.
Mark Pletcher indicated no relevant financial relationships.
Jennifer Lai: Flagship Pioneering – Grant/Research Support. Genfit – Consultant. Novo Nordisk – Advisory Committee/Board Member. Pliant – Grant/Research Support.
Jin Ge, MD, MBA1, Albert Lee, BA1, Oksana Gologorskaya, BS, MS1, Chiung-Yu Huang, PhD1, Mark J.. Pletcher, MD, MPH1, Jennifer C.. Lai, MD, MBA2. P2414 - Characterizing Practice Variations in the Care of Hospitalized Patients With Cirrhosis Across the University of California Health, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
