Monday Poster Session
Category: Liver
P2426 - Mortality Differences in Those Admitted for Sepsis With Comorbid Alcohol Associated Cirrhosis vs Non-Alcohol Associated Cirrhosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Laine A. Lyles, DO
Prisma Health-Midlands / University of South Carolina
Columbia, SC
Presenting Author(s)
Laine A. Lyles, DO1, Eric A. Klingeman, DO2, Brian Haimerl, BS3, William E.. Lyles, MD4
1Prisma Health-Midlands / University of South Carolina, Columbia, SC; 2Prisma Health-Midlands / University of South Carolina, Lexington, SC; 3University of South Carolina School of Medicine-Columbia, Cayce, SC; 4Blount Memorial Hospital, Rockford, TN
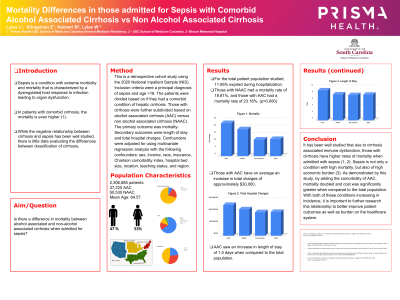
Introduction: Sepsis is a condition with extreme morbidity and mortality that is characterized by a dysregulated host response to infection leading to organ dysfunction. In patients with comorbid cirrhosis, the mortality is even higher (1). While the negative relationship between cirrhosis and sepsis has been well studied, there is little data evaluating the differences between classification of cirrhosis.
Methods: This is a retrospective cohort study using the 2020 National Inpatient Sample (NIS). Inclusion criteria were a principal diagnosis of sepsis and age >18. The patients were divided based on if they had a comorbid condition of hepatic cirrhosis. Those with cirrhosis were further subdivided based on alcohol associated cirrhosis (AAC) versus non alcohol associated cirrhosis (NAAC). The primary outcome was mortality. Secondary outcomes were length of stay and total hospital charges. Confounders were adjusted for using multivariate regression analysis with the following confounders: sex, income, race, insurance, Charlson comorbidity index, hospital bed size, location, teaching status, and region.
Results: 2,306,885 Patients were included in the study, 37,220 of which had alcohol associated cirrhosis, and 50,535 with non alcohol associated cirrhosis. All groups predominantly consisted of Caucasian males in the 6th and 7th decade of life who were treated at large, urban teaching hospitals in the Southern United States. For the total patient population studied, 11.95% expired during hospitalization.Those with NAAC had a mortality rate of 18.81%, and those with AAC had a mortality rate of 23.18%. Additionally, those with AAC have on average an increase in total charges of approximately $30,000, and an increase in length of stay of 1.5 days when compared to the total population.
Discussion: It has been well studied that due to cirrhosis associated immune dysfunction, those with cirrhosis have higher rates of mortality when admitted with sepsis (1, 2). Sepsis is not only a condition with high mortality, but also of high economic burden (3). As demonstrated by this study, by adding the comorbidity of AAC, mortality doubled and cost was significantly greater when compared to the total population. With both of these conditions increasing in incidence, it is important to further research this relationship to better improve patient outcomes as well as burden on the healthcare system.
Disclosures:
Laine A. Lyles, DO1, Eric A. Klingeman, DO2, Brian Haimerl, BS3, William E.. Lyles, MD4. P2426 - Mortality Differences in Those Admitted for Sepsis With Comorbid Alcohol Associated Cirrhosis vs Non-Alcohol Associated Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Prisma Health-Midlands / University of South Carolina, Columbia, SC; 2Prisma Health-Midlands / University of South Carolina, Lexington, SC; 3University of South Carolina School of Medicine-Columbia, Cayce, SC; 4Blount Memorial Hospital, Rockford, TN
Introduction: Sepsis is a condition with extreme morbidity and mortality that is characterized by a dysregulated host response to infection leading to organ dysfunction. In patients with comorbid cirrhosis, the mortality is even higher (1). While the negative relationship between cirrhosis and sepsis has been well studied, there is little data evaluating the differences between classification of cirrhosis.
Methods: This is a retrospective cohort study using the 2020 National Inpatient Sample (NIS). Inclusion criteria were a principal diagnosis of sepsis and age >18. The patients were divided based on if they had a comorbid condition of hepatic cirrhosis. Those with cirrhosis were further subdivided based on alcohol associated cirrhosis (AAC) versus non alcohol associated cirrhosis (NAAC). The primary outcome was mortality. Secondary outcomes were length of stay and total hospital charges. Confounders were adjusted for using multivariate regression analysis with the following confounders: sex, income, race, insurance, Charlson comorbidity index, hospital bed size, location, teaching status, and region.
Results: 2,306,885 Patients were included in the study, 37,220 of which had alcohol associated cirrhosis, and 50,535 with non alcohol associated cirrhosis. All groups predominantly consisted of Caucasian males in the 6th and 7th decade of life who were treated at large, urban teaching hospitals in the Southern United States. For the total patient population studied, 11.95% expired during hospitalization.Those with NAAC had a mortality rate of 18.81%, and those with AAC had a mortality rate of 23.18%. Additionally, those with AAC have on average an increase in total charges of approximately $30,000, and an increase in length of stay of 1.5 days when compared to the total population.
Discussion: It has been well studied that due to cirrhosis associated immune dysfunction, those with cirrhosis have higher rates of mortality when admitted with sepsis (1, 2). Sepsis is not only a condition with high mortality, but also of high economic burden (3). As demonstrated by this study, by adding the comorbidity of AAC, mortality doubled and cost was significantly greater when compared to the total population. With both of these conditions increasing in incidence, it is important to further research this relationship to better improve patient outcomes as well as burden on the healthcare system.
Disclosures:
Laine Lyles indicated no relevant financial relationships.
Eric Klingeman indicated no relevant financial relationships.
Brian Haimerl indicated no relevant financial relationships.
William Lyles indicated no relevant financial relationships.
Laine A. Lyles, DO1, Eric A. Klingeman, DO2, Brian Haimerl, BS3, William E.. Lyles, MD4. P2426 - Mortality Differences in Those Admitted for Sepsis With Comorbid Alcohol Associated Cirrhosis vs Non-Alcohol Associated Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

