Monday Poster Session
Category: Liver
P2442 - Impact of Acute Kidney Injury on Clinical Outcomes of Hepatobiliary Cancer Patients With SARS-COV2 Infection
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall

Sania Saleem, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Ayobami Olafimihan, MD1, Sania Saleem, MD1, Chidiebele Omaliko, MD2, Oghenefejiro Ogwor, MD3, Oluwanifemi Balogun, MD4, Chukwunonso B. Ezeani, MBBS5, Ekrem G. Turk, MD1, Chun-Wei Pan, MD1, Muhammad Bilal Ibrahim, MD1, Seema Gandhi, MD1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 3St. Peters University Hospital, New Brunswick, NJ; 4Albert Einstein Medical Center, Philadelphia, PA; 5Baton Rouge General Hospital, Baton Rouge, LA
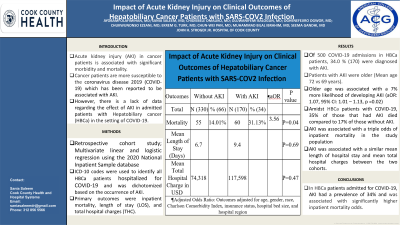
Introduction: Acute kidney injury (AKI) in cancer patients is associated with significant morbidity and mortality. Cancer patients are more susceptible to the coronavirus disease 2019 (COVID-19) which has been reported to be associated with AKI. However, there is a lack of data regarding the effect of AKI in patients with Hepatobiliary cancer (HBCa) in the setting of COVID-19.
Methods: Retrospective cohort analyses were conducted using the National Inpatient Sample (NIS), 2020. Multivariate logistic regression was used to identify predictors and examine the effect of AKI among HBCa patients (hepatocellular carcinoma [HCC], cholangiocarcinoma, and gall bladder cancer) hospitalized for COVID-19.
Results: There was a total of 500 COVID-19 admissions in HBCa patients. Of these, 34.0 % (170) were diagnosed with AKI. Patients with AKI were older (Mean age 72 vs 69 years). Older age was associated with a 7% more likelihood of developing AKI (adjusted odds ratio (AOR): 1.07, 95% confidence interval (CI): 1.01 – 1.13, p =0.02).
Amidst HBCa patients with COVID-19, 35% of those that had AKI died compare to 17% of those without AKI. On multivariate analysis, AKI was associated with a triple risk of inpatient mortality in the study population (AOR: 2.72, 95% CI: 1.03-7.24, p=0.04). AKI was associated with a similar mean length of hospital stay (LOS) between the two cohorts (9.5 vs. 6.8 days, 95% CI: -2.22 - 3.30, p = 0.7). The mean total hospital charges between COVID-19 patients with HBCa who developed AKI and those without AKI were similar ($117,598 vs $74,318, 95% CI: -31,297 - 67,624, p =0.47).
Discussion: In HBCa patients admitted for COVID-19, AKI had a prevalence of 34% and was associated with significantly higher inpatient mortality. LOS and total hospital charges were similar in both study groups. Older age was an independent predictor of COVID-19 related AKI in HBCa patients.
Disclosures:
Ayobami Olafimihan, MD1, Sania Saleem, MD1, Chidiebele Omaliko, MD2, Oghenefejiro Ogwor, MD3, Oluwanifemi Balogun, MD4, Chukwunonso B. Ezeani, MBBS5, Ekrem G. Turk, MD1, Chun-Wei Pan, MD1, Muhammad Bilal Ibrahim, MD1, Seema Gandhi, MD1. P2442 - Impact of Acute Kidney Injury on Clinical Outcomes of Hepatobiliary Cancer Patients With SARS-COV2 Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 3St. Peters University Hospital, New Brunswick, NJ; 4Albert Einstein Medical Center, Philadelphia, PA; 5Baton Rouge General Hospital, Baton Rouge, LA
Introduction: Acute kidney injury (AKI) in cancer patients is associated with significant morbidity and mortality. Cancer patients are more susceptible to the coronavirus disease 2019 (COVID-19) which has been reported to be associated with AKI. However, there is a lack of data regarding the effect of AKI in patients with Hepatobiliary cancer (HBCa) in the setting of COVID-19.
Methods: Retrospective cohort analyses were conducted using the National Inpatient Sample (NIS), 2020. Multivariate logistic regression was used to identify predictors and examine the effect of AKI among HBCa patients (hepatocellular carcinoma [HCC], cholangiocarcinoma, and gall bladder cancer) hospitalized for COVID-19.
Results: There was a total of 500 COVID-19 admissions in HBCa patients. Of these, 34.0 % (170) were diagnosed with AKI. Patients with AKI were older (Mean age 72 vs 69 years). Older age was associated with a 7% more likelihood of developing AKI (adjusted odds ratio (AOR): 1.07, 95% confidence interval (CI): 1.01 – 1.13, p =0.02).
Amidst HBCa patients with COVID-19, 35% of those that had AKI died compare to 17% of those without AKI. On multivariate analysis, AKI was associated with a triple risk of inpatient mortality in the study population (AOR: 2.72, 95% CI: 1.03-7.24, p=0.04). AKI was associated with a similar mean length of hospital stay (LOS) between the two cohorts (9.5 vs. 6.8 days, 95% CI: -2.22 - 3.30, p = 0.7). The mean total hospital charges between COVID-19 patients with HBCa who developed AKI and those without AKI were similar ($117,598 vs $74,318, 95% CI: -31,297 - 67,624, p =0.47).
Discussion: In HBCa patients admitted for COVID-19, AKI had a prevalence of 34% and was associated with significantly higher inpatient mortality. LOS and total hospital charges were similar in both study groups. Older age was an independent predictor of COVID-19 related AKI in HBCa patients.
Disclosures:
Ayobami Olafimihan indicated no relevant financial relationships.
Sania Saleem indicated no relevant financial relationships.
Chidiebele Omaliko indicated no relevant financial relationships.
Oghenefejiro Ogwor indicated no relevant financial relationships.
Oluwanifemi Balogun indicated no relevant financial relationships.
Chukwunonso Ezeani indicated no relevant financial relationships.
Ekrem Turk indicated no relevant financial relationships.
Chun-Wei Pan indicated no relevant financial relationships.
Muhammad Bilal Ibrahim indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Ayobami Olafimihan, MD1, Sania Saleem, MD1, Chidiebele Omaliko, MD2, Oghenefejiro Ogwor, MD3, Oluwanifemi Balogun, MD4, Chukwunonso B. Ezeani, MBBS5, Ekrem G. Turk, MD1, Chun-Wei Pan, MD1, Muhammad Bilal Ibrahim, MD1, Seema Gandhi, MD1. P2442 - Impact of Acute Kidney Injury on Clinical Outcomes of Hepatobiliary Cancer Patients With SARS-COV2 Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
