Monday Poster Session
Category: Liver
P2443 - Impact of Acute Kidney Injury on Alcoholic Hepatitis Hospitalizations: Retrospective Analysis from the National Inpatient Sample Database
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall

Sania Saleem, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Sania Saleem, MD1, Daksh Ahluwalia, MD1, Bashar Attar, MD2, Rohan Gajjar, MD1, Seema Gandhi, MD1, Sultan Mahmood, MD3
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Cook County Health, Chicago, IL; 3Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
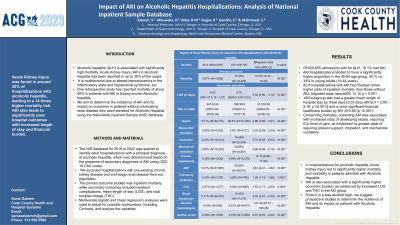
Introduction: Alcoholic hepatitis (ALH) is associated with significantly high mortality, with up to 30% reported Acute Kidney Injury (AKI) rates. Multiple factors can be responsible; altered hemodynamics in the inflammatory state, hepatorenal syndrome, hospitalization, etc. One retrospective study reported mortality of about 40% in patients with AKI in biopsy-proven Alcoholic hepatitis. We aim to determine the incidence of AKI and its impact on outcomes in patients without pre-existing renal disease who were admitted for Alcoholic Hepatitis using the Nationwide Inpatient Sample (NIS) database.
Methods: The NIS database for 2016 to 2020 was queried to identify adult hospitalizations with a principal diagnosis of ALH, which was divided into two cohorts: with and without AKI using (ICD-10-CM) codes. We excluded hospitalizations with pre-existing chronic kidney disease and end-stage renal disease from our population. The primary outcome studied was inpatient mortality, while secondary outcomes included inpatient complications, mean length of stay (LOS), and total hospital charge (THC). Multivariate logistic and linear regression analyses were used to adjust for possible confounders, including Cirrhosis, and analyze the variables.
Results: Of 629,855 admissions for ALH, 19.1% had AKI. AKI hospitalizations tended to have a significantly higher proportion in the 45-64 age group, 55 % vs. 34% in young adults (18-44 years). ALH hospitalizations with AKI had fourteen times higher odds of inpatient mortality than those without AKI; Adjusted odds ratio(aOR) 14.15 p < 0.001. AKI subgroup also had a greater mean length of hospital stay by three days [3.03 days (95%CI = 2.90 – 3.16, p < 0.001)] and a more significant financial healthcare burden by $51,619.58 (p < 0.001). Concerning morbidity, coexisting AKI was associated with increased odds of developing sepsis, requiring ICU level of care, as evidenced by greater odds of requiring pressor support, intubation, and mechanical ventilation.
Discussion: In hospitalizations for alcoholic hepatitis, Acute Kidney Injury led to 14 times higher odds for mortality. There is markedly raised morbidity in patients admitted with Alcoholic Hepatitis, as evidenced by higher odds of sepsis and ICU admissions. AKI is also associated with a significantly higher economic burden, as evidenced by increased LOS and THC in the AKI group. Since it is a less-studied topic, we suggest prospective studies to determine the incidence of AKI and its impact on patients with Alcoholic Hepatitis.
Disclosures:
Sania Saleem, MD1, Daksh Ahluwalia, MD1, Bashar Attar, MD2, Rohan Gajjar, MD1, Seema Gandhi, MD1, Sultan Mahmood, MD3. P2443 - Impact of Acute Kidney Injury on Alcoholic Hepatitis Hospitalizations: Retrospective Analysis from the National Inpatient Sample Database, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Cook County Health, Chicago, IL; 3Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Introduction: Alcoholic hepatitis (ALH) is associated with significantly high mortality, with up to 30% reported Acute Kidney Injury (AKI) rates. Multiple factors can be responsible; altered hemodynamics in the inflammatory state, hepatorenal syndrome, hospitalization, etc. One retrospective study reported mortality of about 40% in patients with AKI in biopsy-proven Alcoholic hepatitis. We aim to determine the incidence of AKI and its impact on outcomes in patients without pre-existing renal disease who were admitted for Alcoholic Hepatitis using the Nationwide Inpatient Sample (NIS) database.
Methods: The NIS database for 2016 to 2020 was queried to identify adult hospitalizations with a principal diagnosis of ALH, which was divided into two cohorts: with and without AKI using (ICD-10-CM) codes. We excluded hospitalizations with pre-existing chronic kidney disease and end-stage renal disease from our population. The primary outcome studied was inpatient mortality, while secondary outcomes included inpatient complications, mean length of stay (LOS), and total hospital charge (THC). Multivariate logistic and linear regression analyses were used to adjust for possible confounders, including Cirrhosis, and analyze the variables.
Results: Of 629,855 admissions for ALH, 19.1% had AKI. AKI hospitalizations tended to have a significantly higher proportion in the 45-64 age group, 55 % vs. 34% in young adults (18-44 years). ALH hospitalizations with AKI had fourteen times higher odds of inpatient mortality than those without AKI; Adjusted odds ratio(aOR) 14.15 p < 0.001. AKI subgroup also had a greater mean length of hospital stay by three days [3.03 days (95%CI = 2.90 – 3.16, p < 0.001)] and a more significant financial healthcare burden by $51,619.58 (p < 0.001). Concerning morbidity, coexisting AKI was associated with increased odds of developing sepsis, requiring ICU level of care, as evidenced by greater odds of requiring pressor support, intubation, and mechanical ventilation.
Discussion: In hospitalizations for alcoholic hepatitis, Acute Kidney Injury led to 14 times higher odds for mortality. There is markedly raised morbidity in patients admitted with Alcoholic Hepatitis, as evidenced by higher odds of sepsis and ICU admissions. AKI is also associated with a significantly higher economic burden, as evidenced by increased LOS and THC in the AKI group. Since it is a less-studied topic, we suggest prospective studies to determine the incidence of AKI and its impact on patients with Alcoholic Hepatitis.
Disclosures:
Sania Saleem indicated no relevant financial relationships.
Daksh Ahluwalia indicated no relevant financial relationships.
Bashar Attar indicated no relevant financial relationships.
Rohan Gajjar indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Sultan Mahmood indicated no relevant financial relationships.
Sania Saleem, MD1, Daksh Ahluwalia, MD1, Bashar Attar, MD2, Rohan Gajjar, MD1, Seema Gandhi, MD1, Sultan Mahmood, MD3. P2443 - Impact of Acute Kidney Injury on Alcoholic Hepatitis Hospitalizations: Retrospective Analysis from the National Inpatient Sample Database, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
