Monday Poster Session
Category: Liver
P2445 - Patients Receiving Simultaneous Liver-Kidney Transplant Have Improved In-Hospital Outcomes Compared to Patients in the Safety Net Pathway
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Richie Manikat, MD
Stanford University School of Medicine
Redwood City, CA
Presenting Author(s)
Award: Outstanding Research Award in the Liver Category (Trainee)
Award: Presidential Poster Award
Richie Manikat, MD, Sudharshan Achalu, BA, Meera Bhargava, MS, Allison Kwong, MD, Xingxing Cheng, MD, Nakia Chung, MD, Paul Kwo, MD
Stanford University School of Medicine, Redwood City, CA
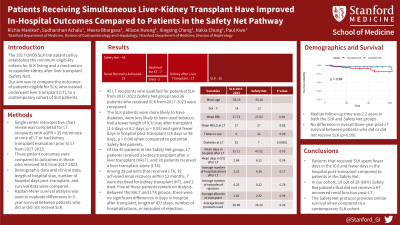
Introduction: The 2017 UNOS Simultaneous Liver-Kidney (SLK) transplant policy establishes the minimum eligibility criteria for SLK listing and a mechanism to expedite kidney after liver transplant (Safety Net). Our AIMS were twofold: 1) to analyze the pre- and post-liver transplant progress of patients eligible for SLK, who instead underwent liver transplant (LT); 2) to compare the outcomes of these patients with a contemporary cohort of SLK patients.
Methods: A single center retrospective chart review was completed for LT recipients with eGFR < 35 ml/min at time of LT or had kidney transplant evaluation prior to LT from 2017-2023. These patient outcomes were compared to outcomes in those who received SLK from 2017-2023. Demographic data and clinical data, length of hospital stay, number of hospital days post-transplant, and survival data were compared. Kaplan-Meier analysis was used to evaluate differences in 3-year survival between patients who did or did not receive SLK.
Results: 45 LT recipients who qualified for potential SLK from 2017-2023 (Safety Net group) and 36 patients who received SLK from 2017-2023 were compared. The SLK patients were more likely to have diabetes, less likely to have used tobacco, had a lower length of ICU stay after transplant (2.6 days vs 6.2 days, p = 0.03) and spent fewer days in hospital post-transplant (25 days vs 48 days, p = 0.04) when compared to potential Safety Net patients (Table).
Of the 45 patients in the Safety Net group, 17 patients received a kidney transplant after a liver transplant (KALT), and 28 patients received a liver transplant alone (LTA). Median follow-up time was 2.2 years in both the SLK and Safety Net groups. No difference was found in overall three-year post-LT survival between patients who did or did not receive SLK (Figure). Among 28 patients that received LTA, 19 achieved renal recovery (defined as eGFR ≥ 35 ml/min) within 12 months, 7 were declined for kidney transplant, and 2 died. Five of these patients remain on dialysis. Between the KALT and LTA groups, there were no significant differences in days in hospital after transplant, length of ICU stays, number of hospitalizations, or episodes of rejection.
Discussion: Patients that received SLK spent fewer days in the ICU and fewer days in the hospital post-transplant compared to patients in the Safety Net. In our cohort, 19 out of 28 patients not receiving KALT recovered renal function post-LT. The Safety Net protocol provides similar survival when compared to a contemporary SLK cohort.

Disclosures:
Richie Manikat, MD, Sudharshan Achalu, BA, Meera Bhargava, MS, Allison Kwong, MD, Xingxing Cheng, MD, Nakia Chung, MD, Paul Kwo, MD. P2445 - Patients Receiving Simultaneous Liver-Kidney Transplant Have Improved In-Hospital Outcomes Compared to Patients in the Safety Net Pathway, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Award: Presidential Poster Award
Richie Manikat, MD, Sudharshan Achalu, BA, Meera Bhargava, MS, Allison Kwong, MD, Xingxing Cheng, MD, Nakia Chung, MD, Paul Kwo, MD
Stanford University School of Medicine, Redwood City, CA
Introduction: The 2017 UNOS Simultaneous Liver-Kidney (SLK) transplant policy establishes the minimum eligibility criteria for SLK listing and a mechanism to expedite kidney after liver transplant (Safety Net). Our AIMS were twofold: 1) to analyze the pre- and post-liver transplant progress of patients eligible for SLK, who instead underwent liver transplant (LT); 2) to compare the outcomes of these patients with a contemporary cohort of SLK patients.
Methods: A single center retrospective chart review was completed for LT recipients with eGFR < 35 ml/min at time of LT or had kidney transplant evaluation prior to LT from 2017-2023. These patient outcomes were compared to outcomes in those who received SLK from 2017-2023. Demographic data and clinical data, length of hospital stay, number of hospital days post-transplant, and survival data were compared. Kaplan-Meier analysis was used to evaluate differences in 3-year survival between patients who did or did not receive SLK.
Results: 45 LT recipients who qualified for potential SLK from 2017-2023 (Safety Net group) and 36 patients who received SLK from 2017-2023 were compared. The SLK patients were more likely to have diabetes, less likely to have used tobacco, had a lower length of ICU stay after transplant (2.6 days vs 6.2 days, p = 0.03) and spent fewer days in hospital post-transplant (25 days vs 48 days, p = 0.04) when compared to potential Safety Net patients (Table).
Of the 45 patients in the Safety Net group, 17 patients received a kidney transplant after a liver transplant (KALT), and 28 patients received a liver transplant alone (LTA). Median follow-up time was 2.2 years in both the SLK and Safety Net groups. No difference was found in overall three-year post-LT survival between patients who did or did not receive SLK (Figure). Among 28 patients that received LTA, 19 achieved renal recovery (defined as eGFR ≥ 35 ml/min) within 12 months, 7 were declined for kidney transplant, and 2 died. Five of these patients remain on dialysis. Between the KALT and LTA groups, there were no significant differences in days in hospital after transplant, length of ICU stays, number of hospitalizations, or episodes of rejection.
Discussion: Patients that received SLK spent fewer days in the ICU and fewer days in the hospital post-transplant compared to patients in the Safety Net. In our cohort, 19 out of 28 patients not receiving KALT recovered renal function post-LT. The Safety Net protocol provides similar survival when compared to a contemporary SLK cohort.

Figure: Kaplan-Meier survival analysis of differences in 3-year survival between patients who did or did not receive SLK
Disclosures:
Richie Manikat indicated no relevant financial relationships.
Sudharshan Achalu indicated no relevant financial relationships.
Meera Bhargava indicated no relevant financial relationships.
Allison Kwong indicated no relevant financial relationships.
Xingxing Cheng indicated no relevant financial relationships.
Nakia Chung indicated no relevant financial relationships.
Paul Kwo indicated no relevant financial relationships.
Richie Manikat, MD, Sudharshan Achalu, BA, Meera Bhargava, MS, Allison Kwong, MD, Xingxing Cheng, MD, Nakia Chung, MD, Paul Kwo, MD. P2445 - Patients Receiving Simultaneous Liver-Kidney Transplant Have Improved In-Hospital Outcomes Compared to Patients in the Safety Net Pathway, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

