Monday Poster Session
Category: Liver
P2446 - A National Database Study: NASH Liver Transplant Has Better 1-year Post-transplant Graft Survival in Comparison to AC and HCV-Related Liver Transplants
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Gina Moon, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Gina Moon, MD1, Tokunbo Ajayi, MD2, Steven Pan, MS1, Sixia Chen, PhD1, Abdul Oseini, MD1, Courtney W. Houchen, MD1
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma City, OK
Introduction: In the year 2022, NASH overtook alcoholic cirrhosis as the leading indication for liver transplants (LTs) in the United States. The aim of this study is to examine the factors that are related to graft and patient survival for the top three indications for LT recipients in the last three decades.
Methods: We retrospectively reviewed the SRTR database for sociodemographic and clinical factors related to graft and patient survival in NASH, alcoholic cirrhosis (AC), and hepatitis C (HCV) LT recipients from 1987 - 2022 in the US. Kaplan-Meier curves and estimated probabilities for graft and patient survival were created for the three indications. Multivariate Cox regressions were conducted with relevant predictors from the following: gender, age, ethnicity, HBV and HCV status, HCC exception criteria, blood type, US citizenship status, payment source, BMI category (< 30 vs. ≥ 30), diabetes status, MELD (< 15 vs. ≥ 15), antiviral therapy, and year of transplant (before or after 2005). P-values < 0.05 were statistically significant.
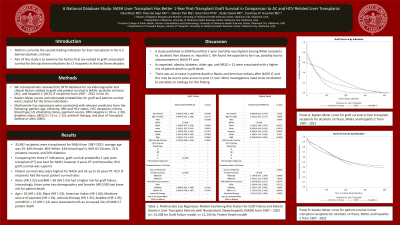
Results: 35,482 recipients were transplanted for NASH from 1987-2022. Average age was 59, 46% female, 80% White, 44% blood type O, 96% US Citizens, 51% privately insured, and 56% diabetics. Comparing the three LT indications, graft survival probability 1 year post-transplant (PT) was best for NASH. However, 3 years PT and thereafter, HCV graft survival was superior. Patient survival rates were highest for NASH and AC up to 10 years PT. HCV LT recipients had the worst patient survival rates. Asian (HR 2.52) and BMI > 30 (HR 1.03) had a higher risk for graft failure. Interestingly, these same two demographics and females (HR 0.90) had lower risk for patient death. Age > 55 (HR 1.43), Black (HR 1.53), American Indian (HR 1.60), Medicare source of payment (HR 1.34), antiviral therapy (HR 1.35), diabetes (HR 1.35), and MELD > 15 (HR 1.12) were associated with an increased risk of NASH LT patient death.
Discussion: A study published in 2009 found that 1-year mortality was highest among NASH recipients vs. alcoholic liver disease vs. hepatitis C. We found the opposite to be true, possibly due to advancements in NASH PT care. As expected, obesity, diabetes, older age, and MELD > 15 were associated with a higher risk of patient death or graft death. There was an increase in patient death in Blacks and American Indians after NASH LT and this may be due to poor access to post LT care. More investigations need to be conducted to elucidate an etiology for this finding.

Disclosures:
Gina Moon, MD1, Tokunbo Ajayi, MD2, Steven Pan, MS1, Sixia Chen, PhD1, Abdul Oseini, MD1, Courtney W. Houchen, MD1. P2446 - A National Database Study: NASH Liver Transplant Has Better 1-year Post-transplant Graft Survival in Comparison to AC and HCV-Related Liver Transplants, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma City, OK
Introduction: In the year 2022, NASH overtook alcoholic cirrhosis as the leading indication for liver transplants (LTs) in the United States. The aim of this study is to examine the factors that are related to graft and patient survival for the top three indications for LT recipients in the last three decades.
Methods: We retrospectively reviewed the SRTR database for sociodemographic and clinical factors related to graft and patient survival in NASH, alcoholic cirrhosis (AC), and hepatitis C (HCV) LT recipients from 1987 - 2022 in the US. Kaplan-Meier curves and estimated probabilities for graft and patient survival were created for the three indications. Multivariate Cox regressions were conducted with relevant predictors from the following: gender, age, ethnicity, HBV and HCV status, HCC exception criteria, blood type, US citizenship status, payment source, BMI category (< 30 vs. ≥ 30), diabetes status, MELD (< 15 vs. ≥ 15), antiviral therapy, and year of transplant (before or after 2005). P-values < 0.05 were statistically significant.
Results: 35,482 recipients were transplanted for NASH from 1987-2022. Average age was 59, 46% female, 80% White, 44% blood type O, 96% US Citizens, 51% privately insured, and 56% diabetics. Comparing the three LT indications, graft survival probability 1 year post-transplant (PT) was best for NASH. However, 3 years PT and thereafter, HCV graft survival was superior. Patient survival rates were highest for NASH and AC up to 10 years PT. HCV LT recipients had the worst patient survival rates. Asian (HR 2.52) and BMI > 30 (HR 1.03) had a higher risk for graft failure. Interestingly, these same two demographics and females (HR 0.90) had lower risk for patient death. Age > 55 (HR 1.43), Black (HR 1.53), American Indian (HR 1.60), Medicare source of payment (HR 1.34), antiviral therapy (HR 1.35), diabetes (HR 1.35), and MELD > 15 (HR 1.12) were associated with an increased risk of NASH LT patient death.
Discussion: A study published in 2009 found that 1-year mortality was highest among NASH recipients vs. alcoholic liver disease vs. hepatitis C. We found the opposite to be true, possibly due to advancements in NASH PT care. As expected, obesity, diabetes, older age, and MELD > 15 were associated with a higher risk of patient death or graft death. There was an increase in patient death in Blacks and American Indians after NASH LT and this may be due to poor access to post LT care. More investigations need to be conducted to elucidate an etiology for this finding.

Figure: Image 1: Panel A - Kaplan-Meier curve for graft survival in liver transplant recipients for alcoholic cirrhosis, NASH, and hepatitis C from 1987 - 2022, log-rank test: p<0.0001. Panel B - Kaplan-Meier curve for patient survival in liver transplant recipients for alcoholic cirrhosis, NASH, and hepatitis C from 1987 - 2022, log-rank test: p<0.0001.
Disclosures:
Gina Moon indicated no relevant financial relationships.
Tokunbo Ajayi indicated no relevant financial relationships.
Steven Pan indicated no relevant financial relationships.
Sixia Chen indicated no relevant financial relationships.
Abdul Oseini indicated no relevant financial relationships.
Courtney Houchen indicated no relevant financial relationships.
Gina Moon, MD1, Tokunbo Ajayi, MD2, Steven Pan, MS1, Sixia Chen, PhD1, Abdul Oseini, MD1, Courtney W. Houchen, MD1. P2446 - A National Database Study: NASH Liver Transplant Has Better 1-year Post-transplant Graft Survival in Comparison to AC and HCV-Related Liver Transplants, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

