Monday Poster Session
Category: Liver
P2447 - Cirrhosis With Ascites in the ED: A QI Project
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- KL
Kevin Lamm, MD
Prisma Health
Greenville, SC
Presenting Author(s)
Kevin Lamm, MD1, Yianni Protopapadakis, MS, DO2, Grant Filowitz, DO1, Gary Abrams, MD1
1Prisma Health, Greenville, SC; 2Prisma Health System, Greenville, SC
Introduction: Ascites is the most common complication of cirrhosis that leads to hospital admission. The prevalence of ascitic fluid infection, most often spontaneous bacterial peritonitis (SBP), at the time of admission in a patient with cirrhosis has been estimated to be 12%. The clinician’s impression that an infection is unlikely does not rule out infection. Mortality due to SBP in hospitalized patients ranges from 10% to 46%. Empiric treatment of suspected infection does not allow for narrowing the spectrum of coverage and typically results in daily administration of antibiotics prescribed for secondary SBP prophylaxis until liver transplant or death. Unnecessary consumption of broad-spectrum antibiotics can lead to microbial resistance and fatal diseases such as Clostridium difficile colitis. Thus, the AASLD recommends that all patients with cirrhosis and ascites emergently admitted to the hospital undergo paracentesis, irrespective of symptoms.
Methods: This retrospective cohort study evaluated patients with cirrhosis and ascites admitted to Greenville Memorial Hospital from Jan 1, 2020 to March 31, 2021. Patients were screened using ICD 10 codes K74, R18 and K70.31. To improve rates of early diagnostic paracentesis we met with the emergency department (ED) quality improvement team for an educational intervention. We then screened for patients using the same criteria from October 1, 2022 to March 31, 2023.
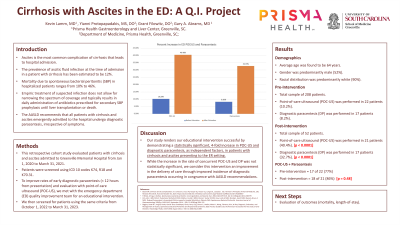
Results: A total of 208 patients were evaluated. This sample featured an average age of 64 years, a 52% male gender predominance, and was predominantly white (90%) and non-Hispanic (98%). The remaining comparative demographics are listed in the table below. Prior to the educational intervention, point-of- care ultrasound (POC-US) was performed in 22 patients (10.2%), and diagnostic paracentesis (DP) in 17 of the 22 (77.3%). After the intervention, a cohort of 52 patients was examined. POC-US was performed in 21/52 (40.4%, p < 0.0001), with 18/21 (85.7%) undergoing DP (p=0.48).
Discussion: This study renders our educational intervention successful by demonstrating a statistically significant, 4-fold increase in POC-US in patients with cirrhosis and ascites admitted into the hospital from the ED. While the rate of DP increase after POC-US was not statistically significant, we consider this intervention an improvement in the delivery of care by greatly increasing the occurrence of diagnostic paracentesis in congruence with AASLD recommendations.

Disclosures:
Kevin Lamm, MD1, Yianni Protopapadakis, MS, DO2, Grant Filowitz, DO1, Gary Abrams, MD1. P2447 - Cirrhosis With Ascites in the ED: A QI Project, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Prisma Health, Greenville, SC; 2Prisma Health System, Greenville, SC
Introduction: Ascites is the most common complication of cirrhosis that leads to hospital admission. The prevalence of ascitic fluid infection, most often spontaneous bacterial peritonitis (SBP), at the time of admission in a patient with cirrhosis has been estimated to be 12%. The clinician’s impression that an infection is unlikely does not rule out infection. Mortality due to SBP in hospitalized patients ranges from 10% to 46%. Empiric treatment of suspected infection does not allow for narrowing the spectrum of coverage and typically results in daily administration of antibiotics prescribed for secondary SBP prophylaxis until liver transplant or death. Unnecessary consumption of broad-spectrum antibiotics can lead to microbial resistance and fatal diseases such as Clostridium difficile colitis. Thus, the AASLD recommends that all patients with cirrhosis and ascites emergently admitted to the hospital undergo paracentesis, irrespective of symptoms.
Methods: This retrospective cohort study evaluated patients with cirrhosis and ascites admitted to Greenville Memorial Hospital from Jan 1, 2020 to March 31, 2021. Patients were screened using ICD 10 codes K74, R18 and K70.31. To improve rates of early diagnostic paracentesis we met with the emergency department (ED) quality improvement team for an educational intervention. We then screened for patients using the same criteria from October 1, 2022 to March 31, 2023.
Results: A total of 208 patients were evaluated. This sample featured an average age of 64 years, a 52% male gender predominance, and was predominantly white (90%) and non-Hispanic (98%). The remaining comparative demographics are listed in the table below. Prior to the educational intervention, point-of- care ultrasound (POC-US) was performed in 22 patients (10.2%), and diagnostic paracentesis (DP) in 17 of the 22 (77.3%). After the intervention, a cohort of 52 patients was examined. POC-US was performed in 21/52 (40.4%, p < 0.0001), with 18/21 (85.7%) undergoing DP (p=0.48).
Discussion: This study renders our educational intervention successful by demonstrating a statistically significant, 4-fold increase in POC-US in patients with cirrhosis and ascites admitted into the hospital from the ED. While the rate of DP increase after POC-US was not statistically significant, we consider this intervention an improvement in the delivery of care by greatly increasing the occurrence of diagnostic paracentesis in congruence with AASLD recommendations.

Figure: Percent increase in POC-US and Paracentesis before and after educational intervention.
Disclosures:
Kevin Lamm indicated no relevant financial relationships.
Yianni Protopapadakis indicated no relevant financial relationships.
Grant Filowitz indicated no relevant financial relationships.
Gary Abrams indicated no relevant financial relationships.
Kevin Lamm, MD1, Yianni Protopapadakis, MS, DO2, Grant Filowitz, DO1, Gary Abrams, MD1. P2447 - Cirrhosis With Ascites in the ED: A QI Project, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
