Monday Poster Session
Category: Liver
P2454 - Transjugular Intrahepatic Portosystemic Shunt Creation for Mechanical Thrombectomy in a Non-Cirrhotic Patient with Extensive Splanchnic Venous Thrombosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Ramon O. Minjares, MD
Underwood Center for Digestive Disorders, Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Ramon O. Minjares, MD1, Michelle Jones-Pauley, DO, MS2, Tamneet Basra, MD2, David W. Victor, MD2, Keshav Menon, MD2, Sudha Kodali, MD, MPH2
1Underwood Center for Digestive Disorders, Houston Methodist Hospital, Houston, TX; 2Houston Methodist Hospital, Houston, TX
Introduction: Acute portomesenteric thrombosis (PMT) can result in worsening symptoms of portal hypertension with potential life-threatening sequelae such as small-bowel (SB) ischemia. Although anticoagulation (AC) is the initial approach, endovascular interventions may be necessary. We present a case of a noncirrhotic patient with extensive PMT who underwent thrombectomy and thrombolysis with successful reduction in clot burden.
Case Description/Methods: A 46-year-old male with asthma presented to the ED with worsening abdominal pain, nausea and bloating. Physical exam was unremarkable. Labs showed Hb 11.8 mg/dL, PLT 297 k/uL, WBC 15.2 k/uL, AST 26 u/L, ALT 32 u/L, ALP 56 u/L, Bilirubin 0.4 mg/dL, INR 1.6, PTT 35.1 sec. CTA revealed extensive thrombus throughout the portal vein, entire splenic vein (SV), and superior mesenteric vein (SMV) in addition to cavernous transformation of the central main portal vein (MPV). The SB had a dusky appearance, suggestive of early ischemic changes. An echocardiogram was normal. Hypercoagulable work-up showed homocysteine 5.8 umol/L, Factor V Laiden (FVL) activity 65%, Protein C 101%, Protein S 67%. The decision was made to pursue mechanical thrombectomy and thrombolysis along with AC given extensive clot burden and concern for gut ischemia.
A transjugular liver biopsy was performed and a TIPS was created. Portogram demonstrated mixed age thrombus in the MPV with cavernous transformation noted in addition to chronic thrombus in the SV and SMV. Pulsed thrombolytic infusion, maceration, and mechanical thrombectomy were performed in the MPV, central SV and SMV. No flow was appreciated in the MPV or the shunt on completion venogram. Two thrombolysis catheters were placed in the SV and SMV for tPA infusion (48 hours). Venograms performed at 24 and 48 hrs showed flow within the MPV with reduction of clot burden.
Patient was found to be homozygous for FVL and prothrombin 20210 mutations. Negative for JAK2 V617F mutation. Flow cytometry was normal. The liver biopsy revealed scant macrovesicular steatosis (< 5%) but no increased fibrosis or inflammation.
Discussion: In extensive PMT, AC alone may not suffice to achieve rapid and stable recanalization. Portal recanalization via TIPS was technically feasible in this noncirrhotic patient and did not result in liver dysfunction. Thrombectomy should be considered in patients with imminent bowel infarction and low likelihood of recanalization following therapeutic AC.

Disclosures:
Ramon O. Minjares, MD1, Michelle Jones-Pauley, DO, MS2, Tamneet Basra, MD2, David W. Victor, MD2, Keshav Menon, MD2, Sudha Kodali, MD, MPH2. P2454 - Transjugular Intrahepatic Portosystemic Shunt Creation for Mechanical Thrombectomy in a Non-Cirrhotic Patient with Extensive Splanchnic Venous Thrombosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Underwood Center for Digestive Disorders, Houston Methodist Hospital, Houston, TX; 2Houston Methodist Hospital, Houston, TX
Introduction: Acute portomesenteric thrombosis (PMT) can result in worsening symptoms of portal hypertension with potential life-threatening sequelae such as small-bowel (SB) ischemia. Although anticoagulation (AC) is the initial approach, endovascular interventions may be necessary. We present a case of a noncirrhotic patient with extensive PMT who underwent thrombectomy and thrombolysis with successful reduction in clot burden.
Case Description/Methods: A 46-year-old male with asthma presented to the ED with worsening abdominal pain, nausea and bloating. Physical exam was unremarkable. Labs showed Hb 11.8 mg/dL, PLT 297 k/uL, WBC 15.2 k/uL, AST 26 u/L, ALT 32 u/L, ALP 56 u/L, Bilirubin 0.4 mg/dL, INR 1.6, PTT 35.1 sec. CTA revealed extensive thrombus throughout the portal vein, entire splenic vein (SV), and superior mesenteric vein (SMV) in addition to cavernous transformation of the central main portal vein (MPV). The SB had a dusky appearance, suggestive of early ischemic changes. An echocardiogram was normal. Hypercoagulable work-up showed homocysteine 5.8 umol/L, Factor V Laiden (FVL) activity 65%, Protein C 101%, Protein S 67%. The decision was made to pursue mechanical thrombectomy and thrombolysis along with AC given extensive clot burden and concern for gut ischemia.
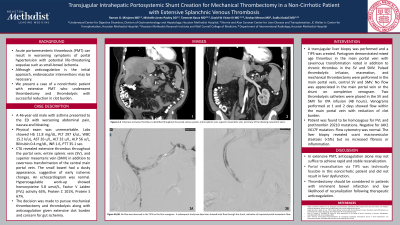
A transjugular liver biopsy was performed and a TIPS was created. Portogram demonstrated mixed age thrombus in the MPV with cavernous transformation noted in addition to chronic thrombus in the SV and SMV. Pulsed thrombolytic infusion, maceration, and mechanical thrombectomy were performed in the MPV, central SV and SMV. No flow was appreciated in the MPV or the shunt on completion venogram. Two thrombolysis catheters were placed in the SV and SMV for tPA infusion (48 hours). Venograms performed at 24 and 48 hrs showed flow within the MPV with reduction of clot burden.
Patient was found to be homozygous for FVL and prothrombin 20210 mutations. Negative for JAK2 V617F mutation. Flow cytometry was normal. The liver biopsy revealed scant macrovesicular steatosis (< 5%) but no increased fibrosis or inflammation.
Discussion: In extensive PMT, AC alone may not suffice to achieve rapid and stable recanalization. Portal recanalization via TIPS was technically feasible in this noncirrhotic patient and did not result in liver dysfunction. Thrombectomy should be considered in patients with imminent bowel infarction and low likelihood of recanalization following therapeutic AC.

Figure: Figure 1A, 1B. No flow was observed in the transjugular intrahepatic portosystemic shunt (TIPS) on the first venogram. A subsequent study two days later showed brisk flow through the shunt, indicative of improved portal-mesenteric flow.
Disclosures:
Ramon Minjares indicated no relevant financial relationships.
Michelle Jones-Pauley indicated no relevant financial relationships.
Tamneet Basra indicated no relevant financial relationships.
David Victor indicated no relevant financial relationships.
Keshav Menon indicated no relevant financial relationships.
Sudha Kodali indicated no relevant financial relationships.
Ramon O. Minjares, MD1, Michelle Jones-Pauley, DO, MS2, Tamneet Basra, MD2, David W. Victor, MD2, Keshav Menon, MD2, Sudha Kodali, MD, MPH2. P2454 - Transjugular Intrahepatic Portosystemic Shunt Creation for Mechanical Thrombectomy in a Non-Cirrhotic Patient with Extensive Splanchnic Venous Thrombosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
