Monday Poster Session
Category: Liver
P2455 - Drug-Induced Liver Injury Masquerading as Choledocholithiasis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Chidiebele E. Omaliko, MD
One Brooklyn Health-Brookdale University Hospital Medical Center
Brooklyn, NY
Presenting Author(s)
Swathi Rajagopal, MD1, Chidiebele Omaliko, MD2, Michael Coles, MD3
1Brookdale Hospital Medical Center, Brooklyn, NY; 2One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 3SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: With nutraceutical consumption becoming ubiquitous, the prevalence of drug induced liver is increasing accordingly. Without FDA regulation, a paucity of data exists on which substances are implicated in DILI and their various metabolic injury patterns.
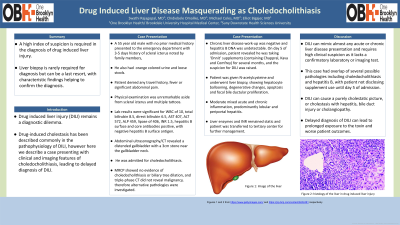
Case Description/Methods: A 55-year-old male with no medical history presented to the hospital with 5 days history of scleral icterus, orange colored urine and loose stools. Patient denied any travel history, fever or significant abdominal pain. Physical examination was unremarkable aside from scleral icterus and multiple tattoos. Lab results were significant for WBC of 10, MCV 87, ferritin 2850, total bilirubin 8.5, direct bilirubin 6.5, AST 407, ALT 572, ALP 459, lipase of 406, INR 1.5, Abdominal ultrasonography/CT revealed a distended gallbladder with a 3cm stone near the gallbladder neck he was admitted for choledocholithiasis. MRCP showed no evidence of choledocholithiasis or biliary tree dilation, and triple-phase CT did not reveal malignancy, therefore alternative pathologies were investigated. Chronic liver disease work-up including autoimmune serology, ceruloplasmin were negative and viral hepatitis panel indicated prior hepatitis B infection. On day 5 of admission, patient revealed he was taking ‘Onnit’ supplements for several months, containing Chappral, Kava and Comfrey, all of which have been implicated in DILI, raising suspicion for DILI. Patient was given N-acetylcysteine and underwent liver biopsy, with hepatocyte ballooning, degenerative changes, apoptosis and focal bile ductular proliferation, moderate acute and chronic inflammation, predominantly lobular and periportal hepatitis, findings somewhat non-specific but which can be seen in DILI. Patient was ultimately transferred to tertiary center for further management. With cessation of the supplements and conservative management the patient continued to convalesce and was ultimately discharged with normalization of liver enzymes.
Discussion: DILI can mimic almost any acute or chronic liver disease presentation and requires high clinical suspicion as it lacks a confirmatory laboratory or imaging test. This case had overlap of several possible pathologies including choledocholithiasis and hepatitis B, with patient not disclosing supplement use until day 5 of admission. DILI can cause a purely cholestatic picture, or cholestasis with hepatitis, bile duct injury or cholangiopathy. Delayed diagnosis of DILI can lead to prolonged exposure to the toxin and worse patient outcomes.
Disclosures:
Swathi Rajagopal, MD1, Chidiebele Omaliko, MD2, Michael Coles, MD3. P2455 - Drug-Induced Liver Injury Masquerading as Choledocholithiasis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brookdale Hospital Medical Center, Brooklyn, NY; 2One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 3SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: With nutraceutical consumption becoming ubiquitous, the prevalence of drug induced liver is increasing accordingly. Without FDA regulation, a paucity of data exists on which substances are implicated in DILI and their various metabolic injury patterns.
Case Description/Methods: A 55-year-old male with no medical history presented to the hospital with 5 days history of scleral icterus, orange colored urine and loose stools. Patient denied any travel history, fever or significant abdominal pain. Physical examination was unremarkable aside from scleral icterus and multiple tattoos. Lab results were significant for WBC of 10, MCV 87, ferritin 2850, total bilirubin 8.5, direct bilirubin 6.5, AST 407, ALT 572, ALP 459, lipase of 406, INR 1.5, Abdominal ultrasonography/CT revealed a distended gallbladder with a 3cm stone near the gallbladder neck he was admitted for choledocholithiasis. MRCP showed no evidence of choledocholithiasis or biliary tree dilation, and triple-phase CT did not reveal malignancy, therefore alternative pathologies were investigated. Chronic liver disease work-up including autoimmune serology, ceruloplasmin were negative and viral hepatitis panel indicated prior hepatitis B infection. On day 5 of admission, patient revealed he was taking ‘Onnit’ supplements for several months, containing Chappral, Kava and Comfrey, all of which have been implicated in DILI, raising suspicion for DILI. Patient was given N-acetylcysteine and underwent liver biopsy, with hepatocyte ballooning, degenerative changes, apoptosis and focal bile ductular proliferation, moderate acute and chronic inflammation, predominantly lobular and periportal hepatitis, findings somewhat non-specific but which can be seen in DILI. Patient was ultimately transferred to tertiary center for further management. With cessation of the supplements and conservative management the patient continued to convalesce and was ultimately discharged with normalization of liver enzymes.
Discussion: DILI can mimic almost any acute or chronic liver disease presentation and requires high clinical suspicion as it lacks a confirmatory laboratory or imaging test. This case had overlap of several possible pathologies including choledocholithiasis and hepatitis B, with patient not disclosing supplement use until day 5 of admission. DILI can cause a purely cholestatic picture, or cholestasis with hepatitis, bile duct injury or cholangiopathy. Delayed diagnosis of DILI can lead to prolonged exposure to the toxin and worse patient outcomes.
Disclosures:
Swathi Rajagopal indicated no relevant financial relationships.
Chidiebele Omaliko indicated no relevant financial relationships.
Michael Coles indicated no relevant financial relationships.
Swathi Rajagopal, MD1, Chidiebele Omaliko, MD2, Michael Coles, MD3. P2455 - Drug-Induced Liver Injury Masquerading as Choledocholithiasis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
