Monday Poster Session
Category: Liver
P2492 - Progressive Multifocal Leukoencephalopathy in Liver Transplant Recipients: A Tale of Two Immunosuppressed Patients
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- DL
Dylan Lopez, MD
Methodist Health System of Dallas
Dallas, TX
Presenting Author(s)
Dylan Lopez, MD1, Wenjing Cai, MD2, Blake Thompson, MD3, Wareef Kabbani, MD4, Mauricio Salicru, MD1, Parvez Mantry, MD5
1Methodist Health System of Dallas, Dallas, TX; 2Methodist Dallas Methodist Center, Dallas, TX; 3Methodist Dallas Medical Center, Dallas, TX; 4Methodist Health System, Dallas, TX; 5Methodist Liver Institute, Dallas, TX
Introduction: Progressive multifocal leukoencephalopathy (PML) is a rare but severe complication that can occur in immunocompromised patients. PML is a demyelinating central nervous system disease caused by the John Cunningham (JC) virus. It can cause neurologic symptoms like cognitive impairment, visual disturbances, and motor deficits. Most commonly seen with AIDS, it can present rarely in solid organ transplant, and very rarely after liver transplant. We present two cases of PML associated with immunosuppressant (IS) medications post-liver transplant.
Case Description/Methods: The first case is a 67-year-old male post-liver transplant with cirrhosis and hepatocellular carcinoma, on IS. He presented two months later with falls and left-sided weakness. Magnetic Resonance Imaging (MRI) showed a subacute infarct within the right frontal corona radiata. He was managed expectantly and discharged to a rehab facility. He returned two months later with complete left-sided hemiparesis, encephalopathy, fever, and suspicious brain MRI findings. Laboratory tests showed pancytopenia and elevated liver functions. Bone marrow biopsy, lumbar puncture, and infectious workup were negative. Brain biopsy revealed PML with JC virus. IS was reduced, with improvement of symptoms.
The second case is a 58-year-old female post-liver transplant with cirrhosis from primary biliary cholangitis. She was discharged with tacrolimus and prednisone. 8 months later she presented with worsening vertigo, left-sided weakness, with MRI showing increased hyperintensity in the cerebellum. She was managed expectantly and discharged to rehab. She returned 10 days later with worsening symptoms and MRI findings. Labs showed pancytopenia, acute kidney injury, and hyperkalemia. She underwent a brain biopsy which showed atypical pleomorphic cells compatible with PML due to JC virus. Her IS was stopped, and intravenous immunoglobulin (IVIG) therapy was started.
Discussion: These cases highlight the significance of considering PML in post-liver transplant patients presenting with neurological changes, with MRI showing hyperintensity in affected regions. As this disease is a disease of exclusion, early diagnosis and prompt reduction of immunosuppression are crucial in managing these conditions, with therapies such as cidofovir and leflunomide showing benefit. Clinicians should have a low threshold for obtaining a brain biopsy and consider PML as a potential cause of neurological changes in post-transplant patients.

Disclosures:
Dylan Lopez, MD1, Wenjing Cai, MD2, Blake Thompson, MD3, Wareef Kabbani, MD4, Mauricio Salicru, MD1, Parvez Mantry, MD5. P2492 - Progressive Multifocal Leukoencephalopathy in Liver Transplant Recipients: A Tale of Two Immunosuppressed Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Methodist Health System of Dallas, Dallas, TX; 2Methodist Dallas Methodist Center, Dallas, TX; 3Methodist Dallas Medical Center, Dallas, TX; 4Methodist Health System, Dallas, TX; 5Methodist Liver Institute, Dallas, TX
Introduction: Progressive multifocal leukoencephalopathy (PML) is a rare but severe complication that can occur in immunocompromised patients. PML is a demyelinating central nervous system disease caused by the John Cunningham (JC) virus. It can cause neurologic symptoms like cognitive impairment, visual disturbances, and motor deficits. Most commonly seen with AIDS, it can present rarely in solid organ transplant, and very rarely after liver transplant. We present two cases of PML associated with immunosuppressant (IS) medications post-liver transplant.
Case Description/Methods: The first case is a 67-year-old male post-liver transplant with cirrhosis and hepatocellular carcinoma, on IS. He presented two months later with falls and left-sided weakness. Magnetic Resonance Imaging (MRI) showed a subacute infarct within the right frontal corona radiata. He was managed expectantly and discharged to a rehab facility. He returned two months later with complete left-sided hemiparesis, encephalopathy, fever, and suspicious brain MRI findings. Laboratory tests showed pancytopenia and elevated liver functions. Bone marrow biopsy, lumbar puncture, and infectious workup were negative. Brain biopsy revealed PML with JC virus. IS was reduced, with improvement of symptoms.
The second case is a 58-year-old female post-liver transplant with cirrhosis from primary biliary cholangitis. She was discharged with tacrolimus and prednisone. 8 months later she presented with worsening vertigo, left-sided weakness, with MRI showing increased hyperintensity in the cerebellum. She was managed expectantly and discharged to rehab. She returned 10 days later with worsening symptoms and MRI findings. Labs showed pancytopenia, acute kidney injury, and hyperkalemia. She underwent a brain biopsy which showed atypical pleomorphic cells compatible with PML due to JC virus. Her IS was stopped, and intravenous immunoglobulin (IVIG) therapy was started.
Discussion: These cases highlight the significance of considering PML in post-liver transplant patients presenting with neurological changes, with MRI showing hyperintensity in affected regions. As this disease is a disease of exclusion, early diagnosis and prompt reduction of immunosuppression are crucial in managing these conditions, with therapies such as cidofovir and leflunomide showing benefit. Clinicians should have a low threshold for obtaining a brain biopsy and consider PML as a potential cause of neurological changes in post-transplant patients.

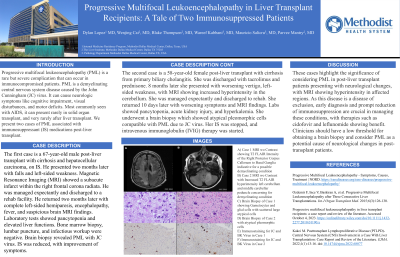
Figure: A) Case 1 MRI wo Contrast showing T2 FLAIR Intensity of the Right Posterior Corpus Callosum to Basal Ganglia indicative for a possible demyelinating condition
B) Case 2 MRI wo Contrast with Increased T2 FLAIR hyperintensity left cerebellum and middle cerebellar peduncle concerning for demyelinating condition
C: Brain Biopsy of Case 1 showing Gemistocytes and glial cells with scattered large atypical cells
D: Brain Biopsy of Case 2 with atypical pleomorphic cells
E: Immunostaining for JC and BK Virus in Case 1
F: Immunostaining for JC and BK Virus in Case 2
B) Case 2 MRI wo Contrast with Increased T2 FLAIR hyperintensity left cerebellum and middle cerebellar peduncle concerning for demyelinating condition
C: Brain Biopsy of Case 1 showing Gemistocytes and glial cells with scattered large atypical cells
D: Brain Biopsy of Case 2 with atypical pleomorphic cells
E: Immunostaining for JC and BK Virus in Case 1
F: Immunostaining for JC and BK Virus in Case 2
Disclosures:
Dylan Lopez indicated no relevant financial relationships.
Wenjing Cai indicated no relevant financial relationships.
Blake Thompson indicated no relevant financial relationships.
Wareef Kabbani indicated no relevant financial relationships.
Mauricio Salicru indicated no relevant financial relationships.
Parvez Mantry indicated no relevant financial relationships.
Dylan Lopez, MD1, Wenjing Cai, MD2, Blake Thompson, MD3, Wareef Kabbani, MD4, Mauricio Salicru, MD1, Parvez Mantry, MD5. P2492 - Progressive Multifocal Leukoencephalopathy in Liver Transplant Recipients: A Tale of Two Immunosuppressed Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
