Monday Poster Session
Category: Liver
P2494 - Dire Dyspnea Dilemma
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- IM
Ivana Martos, MD
Walter Reed National Military Medical Center
Bethesda, Maryland
Presenting Author(s)
Ivana Martos, MD, Muhammad Mansoor, MD, Katharine Salyer, MD
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Diagnosing the cause of dyspnea in a patient with decompensated cirrhosis can be challenging as many diagnoses share overlapping clinical features.
Case Description/Methods: We present a 57-year-old female with decompensated cirrhosis secondary to AIH whose disease course has been complicated by diuretic refractory ascites, encephalopathy, and steroid related pulmonary nocardiosis requiring prolonged antibiotic use.
She presented to a routine outpatient appointment complaining of increasing dyspnea and weight gain. Despite increasing her diuretic dose, the patient was subsequently admitted one week later with worsening symptoms and newly identified hypoxia.
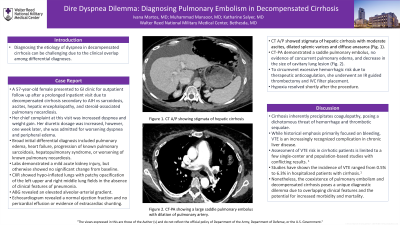
The initial differential diagnosis broadly included cirrhosis related pulmonary edema, new heart failure, hepatopulmonary syndrome, or worsening of known pulmonary nocardiosis despite appropriate antibiotic treatment. Her laboratory evaluation demonstrated a mild acute kidney injury, but otherwise showed no significant change from baseline. A chest radiograph showed hypo-inflated lungs with patchy opacification of the left upper and right middle lung fields. However, the patient was afebrile and lacked clinical features of pneumonia. An arterial blood gas revealed an elevated alveolar-arterial gradient. Her echocardiogram revealed a normal ejection fraction and no pericardial effusion or evidence of extracardiac shunting. A CT-PA demonstrated a saddle pulmonary embolus.. The previously seen cavitary lung lesion had decreased in size and there was no evidence of pulmonary edema. Due to excessive bleeding with therapeutic anticoagulation she underwent an IR guided thrombectomy and IVC filter placement. Her hypoxia resolved shortly after the procedure.
Discussion: A prominent feature of cirrhosis is a disturbance in coagulation with the possibility of bleeding and thrombotic complications. Although a prominent feature of cirrhosis traditionally has been bleeding, venous thromboembolism (VTE) in patients with cirrhosis is an increasingly recognized complication in chronic liver disease. The significance of VTE risk in patients with cirrhosis is limited to a few single-center and population-based studies with conflicting results. However, studies have shown the incidence of VTE ranged from 0.5% to 6.3% in hospitalized patients with cirrhosis. Nonetheless, the coexistence of pulmonary embolism and decompensated cirrhosis poses a unique diagnostic dilemma due to overlapping clinical features and the potential for increased morbidity and mortality.

Disclosures:
Ivana Martos, MD, Muhammad Mansoor, MD, Katharine Salyer, MD. P2494 - Dire Dyspnea Dilemma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Diagnosing the cause of dyspnea in a patient with decompensated cirrhosis can be challenging as many diagnoses share overlapping clinical features.
Case Description/Methods: We present a 57-year-old female with decompensated cirrhosis secondary to AIH whose disease course has been complicated by diuretic refractory ascites, encephalopathy, and steroid related pulmonary nocardiosis requiring prolonged antibiotic use.
She presented to a routine outpatient appointment complaining of increasing dyspnea and weight gain. Despite increasing her diuretic dose, the patient was subsequently admitted one week later with worsening symptoms and newly identified hypoxia.
The initial differential diagnosis broadly included cirrhosis related pulmonary edema, new heart failure, hepatopulmonary syndrome, or worsening of known pulmonary nocardiosis despite appropriate antibiotic treatment. Her laboratory evaluation demonstrated a mild acute kidney injury, but otherwise showed no significant change from baseline. A chest radiograph showed hypo-inflated lungs with patchy opacification of the left upper and right middle lung fields. However, the patient was afebrile and lacked clinical features of pneumonia. An arterial blood gas revealed an elevated alveolar-arterial gradient. Her echocardiogram revealed a normal ejection fraction and no pericardial effusion or evidence of extracardiac shunting. A CT-PA demonstrated a saddle pulmonary embolus.. The previously seen cavitary lung lesion had decreased in size and there was no evidence of pulmonary edema. Due to excessive bleeding with therapeutic anticoagulation she underwent an IR guided thrombectomy and IVC filter placement. Her hypoxia resolved shortly after the procedure.
Discussion: A prominent feature of cirrhosis is a disturbance in coagulation with the possibility of bleeding and thrombotic complications. Although a prominent feature of cirrhosis traditionally has been bleeding, venous thromboembolism (VTE) in patients with cirrhosis is an increasingly recognized complication in chronic liver disease. The significance of VTE risk in patients with cirrhosis is limited to a few single-center and population-based studies with conflicting results. However, studies have shown the incidence of VTE ranged from 0.5% to 6.3% in hospitalized patients with cirrhosis. Nonetheless, the coexistence of pulmonary embolism and decompensated cirrhosis poses a unique diagnostic dilemma due to overlapping clinical features and the potential for increased morbidity and mortality.

Figure: Saddle Pulmonary Embolus discovered on CT
Disclosures:
Ivana Martos indicated no relevant financial relationships.
Muhammad Mansoor: Pfizer – Stock-publicly held company(excluding mutual/index funds). Regeneron – Stock-publicly held company(excluding mutual/index funds).
Katharine Salyer indicated no relevant financial relationships.
Ivana Martos, MD, Muhammad Mansoor, MD, Katharine Salyer, MD. P2494 - Dire Dyspnea Dilemma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
