Monday Poster Session
Category: Liver
P2495 - Recurrent Bacteremia and Cholangitis from Eroded Hepatic Artery Pseudoaneurysm Coil into the Common Bile Duct: A Rare Indication for Liver Transplantation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Supisara Tintara, MD
Keck School of Medicine, University of Southern California
Los Angeles, CA
Presenting Author(s)
Supisara Tintara, MD1, Aileen Bui, MD2, Patrick Chang, MD2, Kambiz Etesami, MD1, Brian Kim, MD1
1Keck School of Medicine, University of Southern California, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: Patients with structural biliary disease have a high risk of bacterial cholangitis with high morbidity. Model for end-stage liver disease (MELD) exception points are provided to patients with severe structural damage of the biliary tree as these patients have limited medical therapies and excellent outcome after liver transplantation (LT).
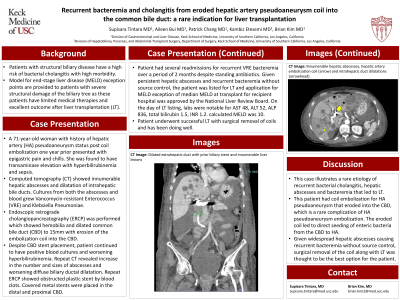
Case Description/Methods: A 71-year-old woman with history of hepatic artery (HA) pseudoaneurysm status post coil embolization one year prior presented with epigastric pain and chills. She was found to have transaminase elevation with hyperbilirubinemia and sepsis. Computed tomography (CT) showed innumerable hepatic abscesses and dilatation of intrahepatic bile ducts (Figure 1). Cultures from both the abscesses and blood grew Vancomycin-resistant Enterococcus (VRE) and Klebsiella Pneumoniae. Endoscopic retrograde cholangiopancreatography (ERCP) was performed which showed hemobilia and dilated common bile duct (CBD) to 15mm with erosion of the embolization coil into the CBD. Despite CBD stent placement, patient continued to have positive blood cultures and worsening hyperbilirubinemia. Repeat CT revealed increase in the number and sizes of abscesses and worsening diffuse biliary ductal dilatation. Repeat ERCP showed obstructed plastic stent by blood clots. Covered metal stents were placed in the distal and proximal CBD. Patient had several readmissions for recurrent VRE bacteremia over a period of 2 months despite standing antibiotics. Given persistent hepatic abscesses and recurrent bacteremia without source control, the patient was listed for LT and application for MELD exception of median MELD at transplant for recipient hospital was approved by the National Liver Review Board. On the day of LT listing, labs were notable for AST 48, ALT 52, ALP 836, total bilirubin 1.5, INR 1.2. Calculated MELD was 10. Patient underwent successful LT with surgical removal of coils and has been doing well.
Discussion: This case illustrates a rare etiology of recurrent bacterial cholangitis, hepatic abscesses and bacteremia that led to LT. This patient had coil embolization for HA pseudoaneurysm that eroded into the CBD, which is a rare complication of HA pseudoaneurysm embolization. The eroded coil led to direct seeding of enteric bacteria from the CBD to HA. Given widespread hepatic abscesses causing recurrent bacteremia without source control, surgical removal of the coil along with LT was thought to be the best option for the patient.

Disclosures:
Supisara Tintara, MD1, Aileen Bui, MD2, Patrick Chang, MD2, Kambiz Etesami, MD1, Brian Kim, MD1. P2495 - Recurrent Bacteremia and Cholangitis from Eroded Hepatic Artery Pseudoaneurysm Coil into the Common Bile Duct: A Rare Indication for Liver Transplantation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Keck School of Medicine, University of Southern California, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: Patients with structural biliary disease have a high risk of bacterial cholangitis with high morbidity. Model for end-stage liver disease (MELD) exception points are provided to patients with severe structural damage of the biliary tree as these patients have limited medical therapies and excellent outcome after liver transplantation (LT).
Case Description/Methods: A 71-year-old woman with history of hepatic artery (HA) pseudoaneurysm status post coil embolization one year prior presented with epigastric pain and chills. She was found to have transaminase elevation with hyperbilirubinemia and sepsis. Computed tomography (CT) showed innumerable hepatic abscesses and dilatation of intrahepatic bile ducts (Figure 1). Cultures from both the abscesses and blood grew Vancomycin-resistant Enterococcus (VRE) and Klebsiella Pneumoniae. Endoscopic retrograde cholangiopancreatography (ERCP) was performed which showed hemobilia and dilated common bile duct (CBD) to 15mm with erosion of the embolization coil into the CBD. Despite CBD stent placement, patient continued to have positive blood cultures and worsening hyperbilirubinemia. Repeat CT revealed increase in the number and sizes of abscesses and worsening diffuse biliary ductal dilatation. Repeat ERCP showed obstructed plastic stent by blood clots. Covered metal stents were placed in the distal and proximal CBD. Patient had several readmissions for recurrent VRE bacteremia over a period of 2 months despite standing antibiotics. Given persistent hepatic abscesses and recurrent bacteremia without source control, the patient was listed for LT and application for MELD exception of median MELD at transplant for recipient hospital was approved by the National Liver Review Board. On the day of LT listing, labs were notable for AST 48, ALT 52, ALP 836, total bilirubin 1.5, INR 1.2. Calculated MELD was 10. Patient underwent successful LT with surgical removal of coils and has been doing well.
Discussion: This case illustrates a rare etiology of recurrent bacterial cholangitis, hepatic abscesses and bacteremia that led to LT. This patient had coil embolization for HA pseudoaneurysm that eroded into the CBD, which is a rare complication of HA pseudoaneurysm embolization. The eroded coil led to direct seeding of enteric bacteria from the CBD to HA. Given widespread hepatic abscesses causing recurrent bacteremia without source control, surgical removal of the coil along with LT was thought to be the best option for the patient.

Figure: CT scan of the abdomen with contrast shows innumerable hepatic abscesses, hepatic artery embolization coil (arrow) and intrahepatic duct dilatations (arrowhead)
Disclosures:
Supisara Tintara indicated no relevant financial relationships.
Aileen Bui indicated no relevant financial relationships.
Patrick Chang indicated no relevant financial relationships.
Kambiz Etesami indicated no relevant financial relationships.
Brian Kim indicated no relevant financial relationships.
Supisara Tintara, MD1, Aileen Bui, MD2, Patrick Chang, MD2, Kambiz Etesami, MD1, Brian Kim, MD1. P2495 - Recurrent Bacteremia and Cholangitis from Eroded Hepatic Artery Pseudoaneurysm Coil into the Common Bile Duct: A Rare Indication for Liver Transplantation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
